Emergency department
An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital or other primary care center.
Several terms redirect here. For other uses, see Accident and Emergency (disambiguation), Emergency room (disambiguation), and Emergency ward (disambiguation).
Due to the unplanned nature of patient attendance, the department must provide initial treatment for a broad spectrum of illnesses and injuries, some of which may be life-threatening and require immediate attention. In some countries, emergency departments have become important entry points for those without other means of access to medical care.
The emergency departments of most hospitals operate 24 hours a day, although staffing levels may be varied in an attempt to reflect patient volume.
History[edit]
Accident services were provided by workmen's compensation plans, railway companies, and municipalities in Europe and the United States by the late mid-nineteenth century, but the world's first specialized trauma care center was opened in 1911 in the United States at the University of Louisville Hospital in Louisville, Kentucky. It was further developed in the 1930s by surgeon Arnold Griswold, who also equipped police and fire vehicles with medical supplies and trained officers to give emergency care while en route to the hospital.[1][2]
Today, a typical hospital has its emergency department in its own section of the ground floor of the grounds, with its own dedicated entrance. As patients can arrive at any time and with any complaint, a key part of the operation of an emergency department is the prioritization of cases based on clinical need.[3] This process is called triage.
Triage is normally the first stage the patient passes through, and consists of a brief assessment, including a set of vital signs, and the assignment of a "chief complaint" (e.g. chest pain, abdominal pain, difficulty breathing, etc.). Most emergency departments have a dedicated area for this process to take place and may have staff dedicated to performing nothing but a triage role. In most departments, this role is fulfilled by a triage nurse, although dependent on training levels in the country and area, other health care professionals may perform the triage sorting, including paramedics and physicians. Triage is typically conducted face-to-face when the patient presents, or a form of triage may be conducted via radio with an ambulance crew; in this method, the paramedics will call the hospital's triage center with a short update about an incoming patient, who will then be triaged to the appropriate level of care.
Most patients will be initially assessed at triage and then passed to another area of the department, or another area of the hospital, with their waiting time determined by their clinical need. However, some patients may complete their treatment at the triage stage, for instance, if the condition is very minor and can be treated quickly, if only advice is required, or if the emergency department is not a suitable point of care for the patient. Conversely, patients with evidently serious conditions, such as cardiac arrest, will bypass triage altogether and move straight to the appropriate part of the department.
The resuscitation area, commonly referred to as "Trauma" or "Resus", is a key area in most departments. The most seriously ill or injured patients will be dealt with in this area, as it contains the equipment and staff required for dealing with immediately life-threatening illnesses and injuries. In such situations, the time in which the patient is treated is crucial. Typical resuscitation staffing involves at least one attending physician, and at least one and usually two nurses with trauma and Advanced Cardiac Life Support training. These personnel may be assigned to the resuscitation area for the entirety of the shift or may be "on call" for resuscitation coverage (i.e. if a critical case presents via walk-in triage or ambulance, the team will be paged to the resuscitation area to deal with the case immediately). Resuscitation cases may also be attended by residents, radiographers, ambulance personnel, respiratory therapists, hospital pharmacists and students of any of these professions depending upon the skill mix needed for any given case and whether or not the hospital provides teaching services.
Patients who exhibit signs of being seriously ill but are not in immediate danger of life or limb will be triaged to "acute care" or "majors", where they will be seen by a physician and receive a more thorough assessment and treatment. Examples of "majors" include chest pain, difficulty breathing, abdominal pain and neurological complaints. Advanced diagnostic testing may be conducted at this stage, including laboratory testing of blood and/or urine, ultrasonography, CT or MRI scanning. Medications appropriate to manage the patient's condition will also be given. Depending on underlying causes of the patient's chief complaint, he or she may be discharged home from this area or admitted to the hospital for further treatment.
Patients whose condition is not immediately life-threatening will be sent to an area suitable to deal with them, and these areas might typically be termed as a prompt care or minors area. Such patients may still have been found to have significant problems, including fractures, dislocations, and lacerations requiring suturing.
Children can present particular challenges in treatment. Some departments have dedicated pediatrics areas, and some departments employ a play therapist whose job is to put children at ease to reduce the anxiety caused by visiting the emergency department, as well as provide distraction therapy for simple procedures.
Many hospitals have a separate area for evaluation of psychiatric problems. These are often staffed by psychiatrists and mental health nurses and social workers. There is typically at least one room for people who are actively a risk to themselves or others (e.g. suicidal).
Fast decisions on life-and-death cases are critical in hospital emergency departments. As a result, doctors face great pressures to overtest and overtreat. The fear of missing something often leads to extra blood tests and imaging scans for what may be harmless chest pains, run-of-the-mill head bumps, and non-threatening stomach aches, with a high cost on the health care system.[4]
Nomenclature in English[edit]
Emergency department became commonly used when emergency medicine was recognized as a medical specialty, and hospitals and medical centres developed departments of emergency medicine to provide services. Other common variations include 'emergency ward', 'emergency centre' or 'emergency unit'.
Accident and emergency (A&E) is deprecated in the United Kingdom but still in common parlance. It is also still in use in Hong Kong.[5][6] Earlier terms such as 'casualty' or 'casualty department' were previously used officially[7][8] and continue to be used informally. The same applies to 'emergency room', 'emerg', or 'ER' in North America, originating when emergency facilities were provided in a single room of the hospital by the department of surgery.
Regardless of naming convention, there is a widespread usage of directional signage in white text on a red background across the world, which indicates the location of the emergency department, or a hospital with such facilities.
Signs on emergency departments may contain additional information. In some American states, there is close regulation of the design and content of such signs. For example, California requires wording such as "Comprehensive Emergency Medical Service" and "Physician On Duty",[9] to prevent persons in need of critical care from presenting to facilities that are not fully equipped and staffed.
In some countries, including the United States and Canada, a smaller facility that may provide assistance in medical emergencies is known as a clinic. Larger communities often have walk-in clinics where people with medical problems that would not be considered serious enough to warrant an emergency department visit can be seen. These clinics often do not operate on a 24-hour basis. Very large clinics may operate as "free-standing emergency centres", which are open 24 hours and can manage a very large number of conditions. However, if a patient presents to a free-standing clinic with a condition requiring hospital admission, he or she must be transferred to an actual hospital, as these facilities do not have the capability to provide inpatient care.
All accident and emergency (A&E) departments throughout the United Kingdom are financed and managed publicly by the National Health Service (NHS of each constituent country: England, Scotland, Wales and Northern Ireland). The term "A&E" is widely recognised and used rather than the full name; it is used on road signs, official documentation,[25] etc.
A&E services are provided to all, without charge. Other NHS medical care, including hospital treatment following an emergency, is free of charge only to all who are "ordinarily resident" in Britain; residency rather than citizenship is the criterion[26] (details on charges vary from country to country).
In England departments are divided into three categories:[27]
Historically, waits for assessment in A&E were very long in some areas of the UK. In October 2002, the Department of Health introduced a four-hour target in emergency departments that required departments in England to assess and treat patients within four hours of arrival, with referral and assessment by other departments if deemed necessary. It was expected that the patients would have physically left the department within the four hours. Present policy is that 95% of all patient cases do not "breach" this four-hour wait. The busiest departments in the UK outside London include University Hospital of Wales in Cardiff, The North Wales Regional Hospital in Wrexham, the Royal Infirmary of Edinburgh and Queen Alexandra Hospital in Portsmouth.
In July 2014, the QualityWatch research programme published in-depth analysis which tracked 41 million A&E attendances from 2010 to 2013.[28] This showed that the number of patients in a department at any one time was closely linked to waiting times, and that crowding in A&E had increased as a result of a growing and ageing population, compounded by the freezing or reduction of A&E capacity. Between 2010/11 and 2012/13 crowding increased by 8%, despite a rise of just 3% in A&E visits, and this trend looks set to continue. Other influential factors identified by the report included temperature (with both hotter and colder weather pushing up A&E visits), staffing and inpatient bed numbers.
A&E services in the UK are often the focus of a great deal of media and political interest, and data on A&E performance is published weekly.[29] However, this is only one part of a complex urgent and emergency care system. Reducing A&E waiting times therefore requires a comprehensive, coordinated strategy across a range of related services.[30]
Many A&E departments are crowded and confusing. Many of those attending are understandably anxious, and some are mentally ill, and especially at night are under the influence of alcohol or other substances. Pearson Lloyd's redesign – 'A Better A&E' – is claimed to have reduced aggression against hospital staff in the departments by 50 per cent. A system of environmental signage provides location-specific information for patients. Screens provide live information about how many cases are being handled and the current status of the A&E department.[31] Waiting times for patients to be seen at A&E were rising in the years leading up to 2020,[32] and were hugely worsened during the COVID-19 pandemic that started in 2020.[33]
In response to the year-on-year increasing pressure on A&E units, followed by the unprecedented effects of the COVID-19 pandemic, the NHS in late 2020 proposed a radical change to handling of urgent and emergency care,[34]
separating "emergency" and "urgent". Emergencies are life-threatening illnesses or accidents which require immediate, intensive treatment. Services that should be accessed in an emergency include ambulance (via 999) and emergency departments. Urgent requirements are for an illness or injury that requires urgent attention but is not a life-threatening situation. Urgent care services include a phone consultation through the NHS111 Clinical Assessment Service, pharmacy advice, out-of-hours GP appointments, and/or referral to an urgent treatment centre (UTC). As part of the response, walk-in Urgent Treatment Centres (UTC) were created.[35][36] People potentially needing A&E treatment are recommended to phone the NHS111 line, which will either book an arrival time for A&E, or recommend a more appropriate procedure.[25] (Information is for England; details may vary in different countries.)
Critical conditions handled[edit]
Cardiac arrest[edit]
Cardiac arrest may occur in the ED/A&E or a patient may be transported by ambulance to the emergency department already in this state. Treatment is basic life support and advanced life support as taught in advanced life support and advanced cardiac life support courses.
Non-emergency use[edit]
Metrics applicable to the ED can be grouped into three main categories, volume, cycle time, and patient satisfaction. Volume metrics including arrivals per hour, percentage of ED beds occupied, and age of patients are understood at a basic level at all hospitals as an indication for staffing requirements. Cycle time metrics are the mainstays of the evaluation and tracking of process efficiency and are less widespread since an active effort is needed to collect and analyze this data. Patient satisfaction metrics, already commonly collected by nursing groups, physician groups, and hospitals, are useful in demonstrating the impact of changes in patient perception of care over time. Since patient satisfaction metrics are derivative and subjective, they are less useful in primary process improvement. Health information exchanges can reduce nonurgent ED visits by supplying current data about admissions, discharges, and transfers to health plans and accountable care organizations, allowing them to shift ED use to primary care settings.[42]
In all primary care trusts there are out of hours medical consultations provided by general practitioners or nurse practitioners.
In the United States, barriers to accessing care contribute to frequent emergency room use.[43] The National Hospital Ambulatory Medical Care Survey looked at the ten most common symptoms for which giving rise to emergency room visits (cough, sore throat, back pain, fever, headache, abdominal pain, chest pain, other pain, shortness of breath, vomiting) and made suggestions as to which would be the most cost-effective choice among virtual care, retail clinic, urgent care, or emergency room. Notably, certain complaints may also be addressed by a telephone call to a person's primary care provider.[44] However, subsequent studies have shown that identifying non-emergency visits based on discharge diagnoses is inaccurate because people commonly present for emergency care for other reasons and are assigned a diagnosis after testing and evaluation.[45]
In the United States, and many other countries, hospitals are beginning to create areas in their emergency rooms for people with minor injuries. These are commonly referred as Fast Track or Minor Care units. These units are for people with non-life-threatening injuries. The use of these units within a department have been shown to significantly improve the flow of patients through a department and to reduce waiting times. Urgent care clinics are another alternative, where patients can go to receive immediate care for non-life-threatening conditions. To reduce the strain on limited ED resources, American Medical Response created a checklist that allows EMTs to identify intoxicated individuals who can be safely sent to detoxification facilities instead.[46]
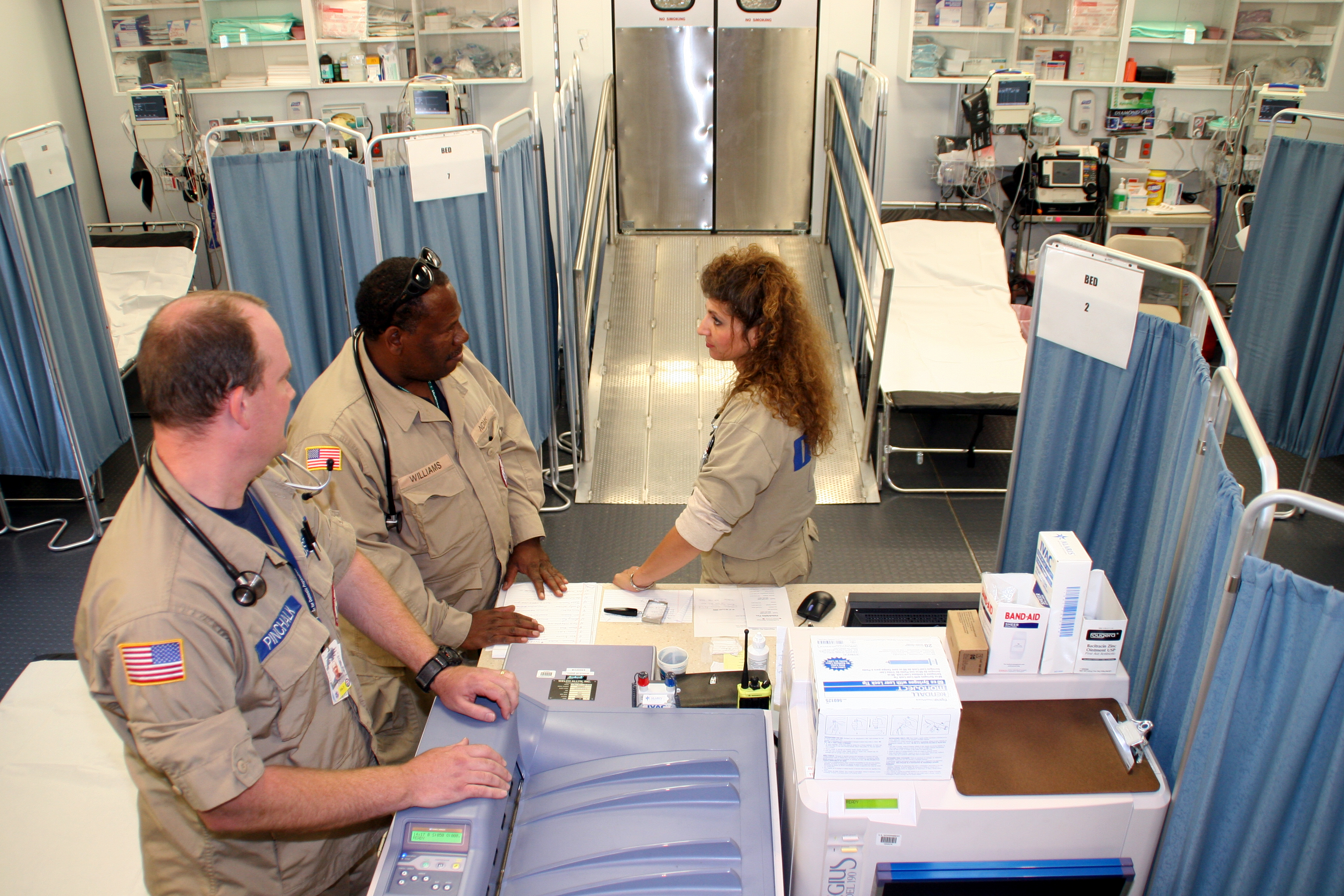
In the military[edit]
Emergency departments in the military benefit from the added support of enlisted personnel who are capable of performing a wide variety of tasks they have been trained for through specialized military schooling. For example, in United States Military Hospitals, Air Force Aerospace Medical Technicians and Navy Hospital Corpsmen perform tasks that fall under the scope of practice of both doctors (i.e. sutures, staples and incision and drainages) and nurses (i.e. medication administration, foley catheter insertion, and obtaining intravenous access) and also perform splinting of injured extremities, nasogastric tube insertion, intubation, wound cauterizing, eye irrigation, and much more. Often, some civilian education and/or certification will be required such as an EMT certification, in case of the need to provide care outside the base where the member is stationed. The presence of highly trained enlisted personnel in an Emergency Departments drastically reduces the workload on nurses and doctors.
Violence against healthcare workers[edit]
According to a survey at an urban inner-city tertiary care center in Vancouver,[63] 57% of health care workers were physically assaulted in 1996. 73% were afraid of patients as a result of violence, 49% hid their identities from patients, and 74% had reduced job satisfaction. Over one-quarter of the respondents took days off because of violence. Of respondents no longer working in the emergency department, 67% reported that they had left the job at least partly owing to violence. Twenty-four-hour security and a workshop on violence prevention strategies were felt to be the most useful potential interventions. Physical exercise, sleep and the company of family and friends were the most frequent coping strategies cited by those surveyed.[63]


