Aminoglycoside
Aminoglycoside is a medicinal and bacteriologic category of traditional Gram-negative antibacterial medications that inhibit protein synthesis and contain as a portion of the molecule an amino-modified glycoside (sugar).[1][2] The term can also refer more generally to any organic molecule that contains amino sugar substructures. Aminoglycoside antibiotics display bactericidal activity against Gram-negative aerobes and some anaerobic bacilli where resistance has not yet arisen but generally not against Gram-positive and anaerobic Gram-negative bacteria.[3]
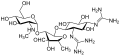
Streptomycin is the first-in-class aminoglycoside antibiotic. It is derived from Streptomyces griseus and is the earliest modern agent used against tuberculosis. Streptomycin lacks the common 2-deoxystreptamine moiety (image right, below) present in most other members of this class. Other examples of aminoglycosides include the deoxystreptamine-containing agents kanamycin, tobramycin, gentamicin, and neomycin (see below).
Aminoglycosides that are derived from bacteria of the Streptomyces genus are named with the suffix -mycin, whereas those that are derived from Micromonospora[4] are named with the suffix -micin.[5] However, this nomenclature system is not specific for aminoglycosides, and so appearance of this set of suffixes does not imply common mechanism of action. (For instance, vancomycin, a glycopeptide antibiotic,[6] and erythromycin,[7] a macrolide antibiotic produced by Saccharopolyspora erythraea, along with its synthetic derivatives clarithromycin and azithromycin, all share the suffixes but have notably different mechanisms of action.)
In the following gallery, kanamycin A to netilmicin are examples of the 4,6-disubstituted deoxystreptamine sub-class of aminoglycosides, the neomycins are examples of the 4,5-disubstituted sub-class, and streptomycin is an example of a non-deoxystreptamine aminoglycoside.[2]
Routes of administration[edit]
Since they are not absorbed from the gut, they are administered intravenously and intramuscularly. Some are used in topical preparations for wounds. Oral administration can be used for gut decontamination (e.g., in hepatic encephalopathy). Tobramycin may be administered in a nebulized form.[15]
Clinical use[edit]
The recent emergence of infections due to Gram-negative bacterial strains with advanced patterns of antimicrobial resistance has prompted physicians to reevaluate the use of these antibacterial agents.[16] This revived interest in the use of aminoglycosides has brought back to light the debate on the two major issues related to these compounds, namely the spectrum of antimicrobial susceptibility and toxicity. Current evidence shows that aminoglycosides do retain activity against the majority of Gram-negative clinical bacterial isolates in many parts of the world. Still, the relatively frequent occurrence of nephrotoxicity and ototoxicity during aminoglycoside treatment makes physicians reluctant to use these compounds in everyday practice. Recent advances in the understanding of the effect of various dosage schedules of aminoglycosides on toxicity have provided a partial solution to this problem, although more research still needs to be done in order to overcome this problem entirely.[17]
Aminoglycosides are in pregnancy category D,[18] that is, there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
Adverse effects[edit]
Aminoglycosides can cause inner ear toxicity which can result in sensorineural hearing loss.[19] The incidence of inner ear toxicity varies from 7 to 90%, depending on the types of antibiotics used, susceptibility of the patient to such antibiotics, and the duration of antibiotic administration.[20]
Another serious and disabling side effect of aminoglycoside use is vestibular ototoxicity.[19] This leads to oscillopsia (gaze instability) and balance impairments that impact all aspects of an individual's antigravity function. This loss is permanent and can happen at any dose.[21][22][23][24]
Frequent use of aminoglycosides could result in kidney damage (Acute kidney injury), that could lead to chronic kidney disease.[25]
Contraindication for specific diseases[edit]
Aminoglycosides can exacerbate weakness in patients with myasthenia gravis, and use is therefore avoided in these patients.[26]
Aminoglycosides are contraindicated in patients with mitochondrial diseases as they may result in impaired mtDNA translation, which can lead to irreversible hearing loss, tinnitus, cardiac toxicity, and renal toxicity. However, hearing loss and tinnitus have also been observed in some patients without mitochondrial diseases.[27]