Antibiotic misuse
Antibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse or overuse of antibiotics, with potentially serious effects on health. It is a contributing factor to the development of antibiotic resistance, including the creation of multidrug-resistant bacteria, informally called "super bugs": relatively harmless bacteria (such as Staphylococcus, Enterococcus and Acinetobacter) can develop resistance to multiple antibiotics and cause life-threatening infections.[1]
History of antibiotic regulation[edit]
Antibiotics have been around since 1928 when penicillin was discovered by Alexander Fleming. In the 1980s, antibiotics that were determined medically important for treatment of animals could be approved under veterinary oversight. In 1996, the National Antimicrobial Resistance Monitoring System (NARMS) was established.[2] Starting in 2010, publications regarding antimicrobial drugs in food became an annual report. Starting in 2012, there was publicly solicited input on how data is to be collected and reported for matters relating to the use of antimicrobials for food-producing animals. Resulting from this, the FDA revised its sampling structure within NARMS with the goal of obtaining more representative livestock data for the key organisms under surveillance.[2] "NARMS partners at CDC and USDA have published over 150 peer-reviewed research articles examining the nature and magnitude of antimicrobial resistance hazards associated with antibiotic use in food-producing animals." In 2014, the FDA began working with the United States Department of Agriculture (USDA) and the Centers of Disease Control and Prevention (CDC) to explore additional mechanisms to obtain data that is representative of antibiotic use in food-producing animals. In 2015, the FDA issued the Veterinary Feed Directive (VFD) final rule, under which veterinarians must authorize the use of antimicrobials within feed for the animals they serve.[2]
In addition to antibiotic regulation in food production, there have been numerous policies put in place to regulate antibiotic distribution in healthcare, specifically in hospital settings. In 2014, the CDC officially recognized the need for antimicrobial stewardship within all U.S. hospitals in their publication of the Core Elements of Hospital Antibiotic Stewardship Programs. These programs outline opportunities for reducing unnecessary antibiotic usage, and provide guidelines for antibiotic prescription for common infections. The CDC highlighted post-prescription tactics for antibiotic regulation, such as reassessing dosages and the class or type of antibiotic used, in order to optimally treat each infection.[3] The CDC also emphasized the need for evidence-based prescribing, a practice that focuses on the utilization of evidence and research to make informed medical decisions;[4] these sentiments were echoed by the American Dental Association (ADA) which works to provide detailed guidelines for dentists considering prescribing their patients antibiotics.[5] In 2019, the CDC published a report concerning the issue and updating the public on the effectiveness of past policy. This report, titled Antibiotic Resistance Threats in the United States, 2019, indicated which pathogens posed the greatest threat of resistance, and highlighted the importance of infection prevention, providing recommendations for prevention strategies.[6]
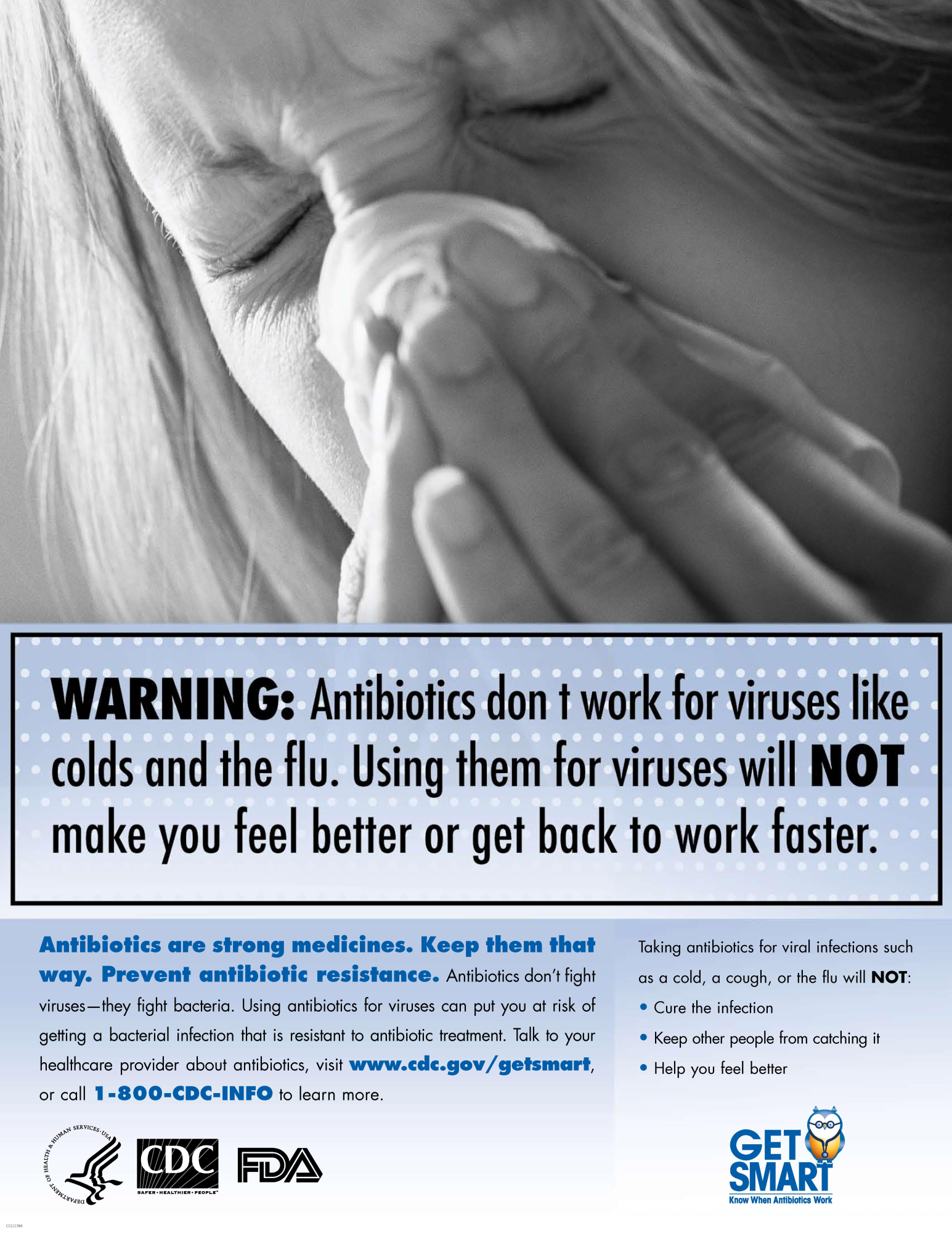
There has also been a substantial effort to educate not only prescribers, but patients too on the issue of antibiotic misuse. The World Health Organization (WHO) has designated a "World Antimicrobial Awareness Week" in November. In 2021, the week's theme was "Spread Awareness, Stop Resistance" and the organization published many different forms of media including podcasts, articles, and infographics to raise awareness for the issue.[7] In the United States, the CDC has published posters and other materials for the purpose of educating the public on antibiotic resistance.[8] State health departments, such as Colorado's Department of Public Health & Environment, have partnered with the CDC to distribute these materials to healthcare providers.[9]
Antibiotics treats bacterial infections rather than viral infections.
Common situations in which antibiotics are overused include the following:[10]
Social and economic impact of antibiotic misuse[edit]
Antibiotics can cause severe reactions and add significantly to the cost of care.[21] In the United States, antibiotics and anti-infectives are the leading cause of adverse effect from drugs. In a study of 32 States in 2011, antibiotics and anti-infectives accounted for nearly 24 percent of ADEs that were present on admission, and 28 percent of those that occurred during a hospital stay.[22]
If antimicrobial resistance continues to increase from current levels, it is estimated that by 2050 ten million people would die every year due to lack of available treatment[23] and the world's GDP would be 2 – 3.5% lower in 2050.[24] If worldwide action is not taken to combat antibiotic misuse and the development of antimicrobial resistance, from 2014 – 2050 it is estimated that 300 million people could die prematurely due to drug resistance and $60 – 100 trillion of economic output would be lost.[24] If the current worldwide development of antimicrobial resistance is delayed by just 10 years, $65 trillion of the world's GDP output can be saved from 2014 to 2050.[24]
Prescribing by an infectious disease specialist compared with prescribing by a non-infectious disease specialist decreases antibiotic consumption and reduces costs.[25]