Chronic pancreatitis
Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions.[1] It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis.[6][7] Tobacco smoke and alcohol misuse are two of the most frequently implicated causes, and the two risk factors are thought to have a synergistic effect with regards to the development of chronic pancreatitis.[4] Chronic pancreatitis is a risk factor for the development of pancreatic cancer.[4]
Chronic pancreatitis
Pancreatitis – chronic – discharge[1]
Exocrine pancreatic insufficiency, Endocrine pancreatic insufficiency (Type 3c diabetes), pancreatic pseudocyst,[4] pancreatic cancer,[4] vitamin deficiency (fat-soluble vitamins)[4]
Alcohol(ism), Immune disorder[5]
Serum trypsinogen, Fecal fat test[2]
Pain medicines, avoiding alcohol(and smoking), among other possible management efforts[2]
50 per 100,000 persons (prevalence)
There have been three symptom profiles described in those with chronic pancreatitis. Type A involves intermittent, severe symptom flare-ups with or without objective pancreatitis amongst a background of symptom-free periods. The type A symptom profile is usually more common early in the course of chronic pancreatitis.[4] Type B chronic pancreatitis involves chronic pain accompanied by intermittent severe attacks.[4] And, the type C symptom profile of chronic pancreatitis involves chronic, long-term, severe pain without interspersed acute flare-ups or symptom exacerbations.[4]
Diagnosis[edit]
The diagnosis of chronic pancreatitis is made based on the history and characteristics of symptoms combined with findings on radiologic imaging.[4] Serum amylase and lipase may be moderately elevated in cases of chronic pancreatitis.
Symptoms of diarrhea, with oily, bulky, and foul-smelling stools indicated steatorrhea or fat malabsorption due to exocrine pancreatic insufficiency. Exocrine pancreatic insufficiency can be confirmed by also checking a fecal elastase level, with low levels specifying exocrine pancreatic insufficiency.[4] A quantitative fecal fat test can also be done to quantify the fat levels in the stool and confirm the presence of exocrine pancreatic insufficiency.[4]
When chronic pancreatitis is caused by genetic factors, elevations in ESR, IgG4, rheumatoid factor, ANA and anti-smooth muscle antibody may be detected.[11]
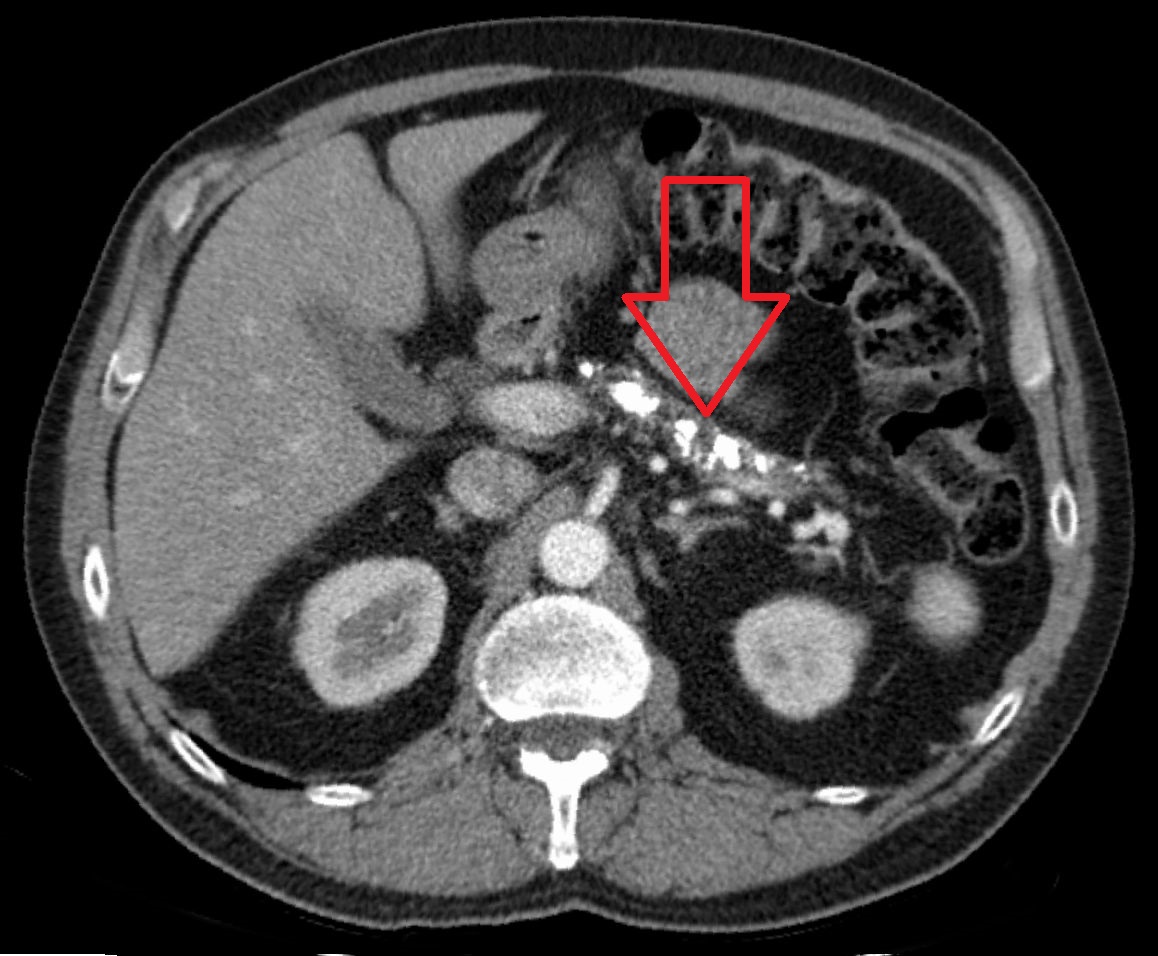
Computed tomography, magnetic resonance cholangiopancreatography (MRCP), and endoscopic ultrasound (EUS) all have similar sensitivity and specificity for diagnosing chronic pancreatitis.[4] MRCP is particularly utilized for its sensitivity in imaging the pancreatic ducts and bile ducts for associated changes such as stones or strictures.[4][12]
A biopsy of the pancreas is not required for the diagnosis.[4] On imaging, pancreatic and bile duct dilatation, atrophy of the pancreas, multiple calcifications of the pancreas, and enlargement of pancreatic glands can be found.[12]
On MRI scan, there is a low T1 signal due to inflammation, fibrosis, focal lesions, and calcifications. In those who are given a contrast agent, there would be a higher T1 signal with late gadolinium enhancement due to compression from the fibrotic areas. The overall thickness of the pancreas will be reduced.[12]
Epidemiology[edit]
The annual incidence of chronic pancreatitis is 5 to 12 per 100,000 persons, the prevalence is 50 per 100,000 persons.[18] It has been reported that the pancreas is able to absorb radioactive cesium (Cs-134 and Cs-137) in great quantities from environmental contamination, causing chronic pancreatitis and probably pancreatic cancer with damage of pancreatic islets with Type 3c (pancreatogenic) diabetes.[19]