Peptic ulcer disease
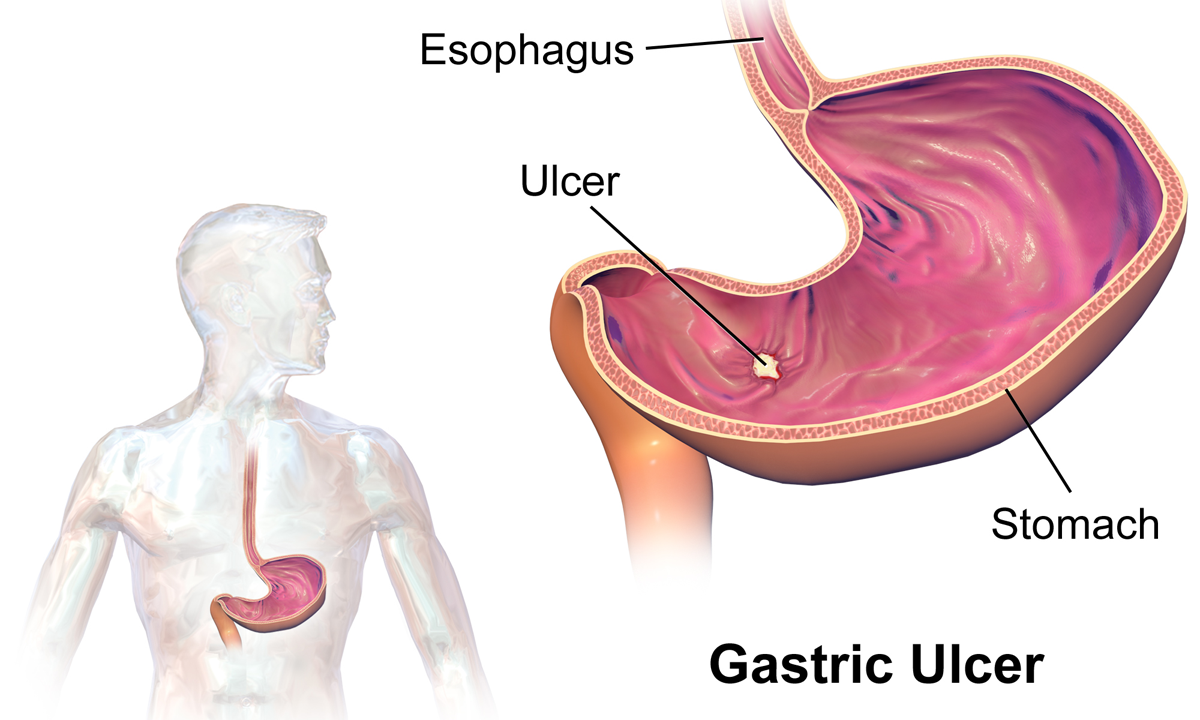
Peptic ulcer disease is a break in the inner lining of the stomach, the first part of the small intestine, or sometimes the lower esophagus.[1][7] An ulcer in the stomach is called a gastric ulcer, while one in the first part of the intestines is a duodenal ulcer.[1] The most common symptoms of a duodenal ulcer are waking at night with upper abdominal pain, and upper abdominal pain that improves with eating.[1] With a gastric ulcer, the pain may worsen with eating.[8] The pain is often described as a burning or dull ache.[1] Other symptoms include belching, vomiting, weight loss, or poor appetite.[1] About a third of older people with peptic ulcers have no symptoms.[1] Complications may include bleeding, perforation, and blockage of the stomach.[2] Bleeding occurs in as many as 15% of cases.[2]
Peptic ulcer disease
Peptic ulcer, stomach ulcer, gastric ulcer, duodenal ulcer
Helicobacter pylori bacteria, non-steroidal anti-inflammatory drugs (NSAIDs), tobacco smoking, Crohn's disease[1][3]
Based on symptoms, confirmed by endoscopy or barium swallow[1]
Medications,[1] stopping NSAIDs, stopping smoking, stopping alcohol consumption
87.4 million (2015)[5]
267,500 (2015)[6]
Common causes include infection with Helicobacter pylori and non-steroidal anti-inflammatory drugs (NSAIDs).[1] Other, less common causes include tobacco smoking, stress as a result of other serious health conditions, Behçet's disease, Zollinger–Ellison syndrome, Crohn's disease, and liver cirrhosis.[1][3] Older people are more sensitive to the ulcer-causing effects of NSAIDs.[1] The diagnosis is typically suspected due to the presenting symptoms with confirmation by either endoscopy or barium swallow.[1] H. pylori can be diagnosed by testing the blood for antibodies, a urea breath test, testing the stool for signs of the bacteria, or a biopsy of the stomach.[1] Other conditions that produce similar symptoms include stomach cancer, coronary heart disease, and inflammation of the stomach lining or gallbladder inflammation.[1]
Diet does not play an important role in either causing or preventing ulcers.[9] Treatment includes stopping smoking, stopping use of NSAIDs, stopping alcohol, and taking medications to decrease stomach acid.[1] The medication used to decrease acid is usually either a proton pump inhibitor (PPI) or an H2 blocker, with four weeks of treatment initially recommended.[1] Ulcers due to H. pylori are treated with a combination of medications, such as amoxicillin, clarithromycin, and a PPI.[4] Antibiotic resistance is increasing and thus treatment may not always be effective.[4] Bleeding ulcers may be treated by endoscopy, with open surgery typically only used in cases in which it is not successful.[2]
Peptic ulcers are present in around 4% of the population.[1] New ulcers were found in around 87.4 million people worldwide during 2015.[5] About 10% of people develop a peptic ulcer at some point in their life.[10] Peptic ulcers resulted in 267,500 deaths in 2015, down from 327,000 in 1990.[6][11] The first description of a perforated peptic ulcer was in 1670, in Princess Henrietta of England.[2] H. pylori was first identified as causing peptic ulcers by Barry Marshall and Robin Warren in the late 20th century,[4] a discovery for which they received the Nobel Prize in 2005.[12]
Cause[edit]
H. pylori[edit]
Helicobacter pylori is one of the major causative factors of peptic ulcer disease. It secretes urease to create an alkaline environment, which is suitable for its survival. It expresses blood group antigen-binding adhesin (BabA) and outer inflammatory protein adhesin (OipA), which enables it to attach to the gastric epithelium. The bacterium also expresses virulence factors such as CagA and PicB, which cause stomach mucosal inflammation. The VacA gene encodes for vacuolating cytotoxin, but its mechanism of causing peptic ulcers is unclear. Such stomach mucosal inflammation can be associated with hyperchlorhydria (increased stomach acid secretion) or hypochlorhydria (reduced stomach acid secretion). Inflammatory cytokines inhibit the parietal cell acid secretion. H. pylori also secretes certain products that inhibit hydrogen potassium ATPase; activate calcitonin gene-related peptide sensory neurons, which increases somatostatin secretion to inhibit acid production by parietal cells; and inhibit gastrin secretion. This reduction in acid production causes gastric ulcers.[16] On the other hand, increased acid production at the pyloric antrum is associated with duodenal ulcers in 10% to 15% of H. pylori infection cases. In this case, somatostatin production is reduced and gastrin production is increased, leading to increased histamine secretion from the enterochromaffin cells, thus increasing acid production. An acidic environment at the antrum causes metaplasia of the duodenal cells, causing duodenal ulcers.[16]
Human immune response toward the bacteria also determines the emergence of peptic ulcer disease. The human IL1B gene encodes for Interleukin 1 beta, and other genes that encode for tumour necrosis factor (TNF) and Lymphotoxin alpha also play a role in gastric inflammation.[16]
NSAIDs[edit]
Taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin[25] can increase the risk of peptic ulcer disease by four times compared to non-users. The risk of getting a peptic ulcer is two times for aspirin users. Risk of bleeding increases if NSAIDs are combined with selective serotonin reuptake inhibitor (SSRI), corticosteroids, antimineralocorticoids, and anticoagulants. The gastric mucosa protects itself from gastric acid with a layer of mucus, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of cyclooxygenase 1 (COX-1), which is essential for the production of these prostaglandins. Besides this, NSAIDs also inhibit stomach mucosa cells proliferation and mucosal blood flow, reducing bicarbonate and mucus secretion, which reduces the integrity of the mucosa. Another type of NSAIDs, called COX-2 selective anti-inflammatory drugs (such as celecoxib), preferentially inhibit COX-2, which is less essential in the gastric mucosa. This reduces the probability of getting peptic ulcers; however, it can still delay ulcer healing for those who already have a peptic ulcer.[16] Peptic ulcers caused by NSAIDs differ from those caused by H. pylori as the latter's appear as a consequence of inflammation of the mucosa (presence of neutrophil and submucosal edema), the former instead as a consequence of a direct damage of the NSAID molecule against COX enzymes, altering the hydrophobic state of the mucus, the permeability of the lining epithelium and mitochondrial machinery of the cell itself. In this way NSAID's ulcers tend to complicate faster and dig deeper in the tissue causing more complications, often asymptomatically until a great portion of the tissue is involved.[26][27]
Stress[edit]
Stress due to serious health problems, such as those requiring treatment in an intensive care unit, is well described as a cause of peptic ulcers, which are also known as stress ulcers.[3]
While chronic life stress was once believed to be the main cause of ulcers, this is no longer the case.[28] It is, however, still occasionally believed to play a role.[28] This may be due to the well-documented effects of stress on gastric physiology, increasing the risk in those with other causes, such as H. pylori or NSAID use.[29]
Diet[edit]
Dietary factors, such as spice consumption, were hypothesized to cause ulcers until the late 20th century, but have been shown to be of relatively minor importance.[30] Caffeine and coffee, also commonly thought to cause or exacerbate ulcers, appear to have little effect.[31][32] Similarly, while studies have found that alcohol consumption increases risk when associated with H. pylori infection, it does not seem to independently increase risk. Even when coupled with H. pylori infection, the increase is modest in comparison to the primary risk factor.[33][34][nb 1]
Other[edit]
Other causes of peptic ulcer disease include gastric ischaemia, drugs, metabolic disturbances, cytomegalovirus (CMV), upper abdominal radiotherapy, Crohn's disease, and vasculitis.[16] Gastrinomas (Zollinger–Ellison syndrome), or rare gastrin-secreting tumors, also cause multiple and difficult-to-heal ulcers.[35]
It is still unclear whether smoking increases the risk of getting peptic ulcers.[16]
Prevention[edit]
Prevention of peptic ulcer disease for those who are taking NSAIDs (with low cardiovascular risk) can be achieved by adding a proton pump inhibitor (PPI), an H2 antagonist, or misoprostol.[16] NSAIDs of the COX-2 inhibitors type may reduce the rate of ulcers when compared to non-selective NSAIDs.[16] PPI is the most popular agent in peptic ulcer prevention.[16] However, there is no evidence that H2 antagonists can prevent stomach bleeding for those taking NSAIDs.[16] Although misoprostol is effective in preventing peptic ulcer, its properties of promoting abortion and causing gastrointestinal distress limit its use.[16] For those with high cardiovascular risk, naproxen with PPI can be a useful choice.[16] Otherwise, low-dose aspirin, celecoxib, and PPI can also be used.[16]