Sjögren syndrome
Sjögren syndrome or Sjögren's syndrome (SjS, SS) is a long-term autoimmune disease that primarily affects the body's exocrine glands, particularly the lacrimal and salivary glands.[4][8] Common symptoms include dry mouth, dry eyes and often seriously affects other organ systems, such as the lungs, kidneys, and nervous system.[9]
Not to be confused with Sjögren–Larsson syndrome and Marinesco–Sjögren syndrome.Sjögren's syndrome
Sjögren's syndrome, sicca syndrome
- UK: /ˈʃɜːɡrɛn/, US: /ˈʃoʊɡrɛn/[1]
Swedish: [ˈɧø̂ːɡreːn]
Long term[4]
Autoimmune disease (unknown cause)[4]
Tissue biopsy, blood tests[2]
Medication side effect, anxiety, sarcoidosis, amyloidosis[5]
Artificial tears, medications to reduce inflammation, surgery[4]
Normal life expectancy[6]
~0.7%[7]
Symptoms[edit]
Overview and importance to patients[edit]
In a 2021 poll of Sjogren's patients, a majority of respondents stated that eight Sjogren's symptoms had a major or moderate impact on their life: fatigue (79%); dry eyes (75%); dry mouth (73%); joint pain (65%); trouble sleeping (64%); eye discomfort (60%); muscle pain (56%); and brain fog (54%).[10][11][12]
Symptoms[edit]
Primary symptoms are dryness (dry mouth and dry eyes[2]), pain and fatigue.[13] Other symptoms can include dry skin, vaginal dryness, a chronic cough, numbness in the arms and legs, feeling tired, muscle and joint pains, and thyroid problems.[4] Those affected are also at an increased risk (15%) of lymphoma.[2][7]
Prevention[edit]
No prevention mechanism exists for Sjögren's syndrome (SS) because of its complexity as an autoimmune disorder.
However lifestyle changes can reduce the risk factors related to developing SS or reduce the severity of the condition for patients who have already been diagnosed.
Diet is strongly associated with the inflammation seen in many autoimmune related diseases, including SS. An experimental study concluded that SS patients often show high sensitivity to gluten that directly relates to inflammation.[71]
Moderate exercise is also helpful in SS patients, mainly reducing the effect of lung inflammation.[72]
Treatment[edit]
Overview[edit]
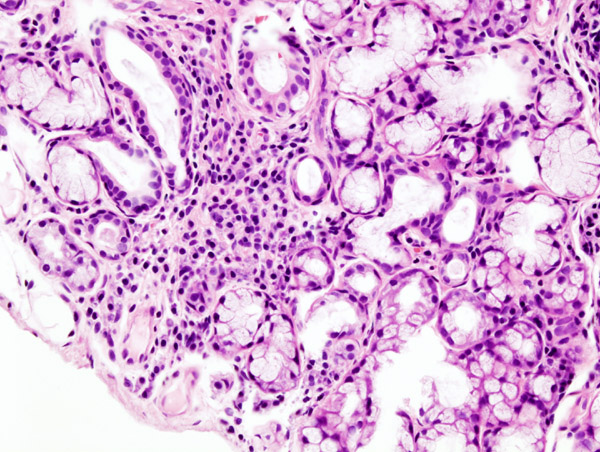
Treatment is directed at managing the person's symptoms.[4] For dry eyes, artificial tears; medications to reduce inflammation; punctal plugs or other surgery to shut the tear ducts may be tried.[4] For a dry mouth, chewing gum (preferably sugar-free); sipping water; or a saliva substitute may be used.[4] In those with joint or muscle pain, ibuprofen may be used.[4] Medications that can cause dryness, such as antihistamines, may also be stopped.[4] The most specific extant diagnostic test requires lip biopsy.
Epidemiology[edit]
Sjögren's syndrome (SS) is the third-most common rheumatic autoimmune disorder, behind rheumatoid arthritis and systemic lupus erythematosus.[17]
There are no geographical differences in the rates of SS.[93] Sjögren's syndrome has been reported in all areas of the world, although regional rates have not been well studied.[93][94]
Depending on the criteria for determining prevalence, studies estimate the prevalence of SS at between 500,000 and two million people in the United States. Broader studies of SS prevalence range widely, with some reports of up to a prevalence of 3% of the population.[17] A few studies have reported that the incidence of the syndrome varies between three and six per 100,000 per year.[17][95]
Between 0.2 and 1.2% of the population is affected, with half having the primary form and half the secondary form.[7] It is around 10 times more common in women than in men.[3] Though the disease commonly begins in middle age, people of any age can be affected.[2][3]
Nine out of 10 SS patients are women.[30][94] In addition to prevalence in women, having a first-degree relative with an autoimmune disease and previous pregnancies have been identified as epidemiological risk factors.[96] Despite the lower risk for men, primary SS in men tends to represent a more severe form of the disease.[97] The role of race and ethnicity in the prevalence of the disease is unknown.
Although Sjögren's syndrome occurs in all age groups, the average age of onset is between ages 40 and 60, although as many as half of all cases may be left undiagnosed or unreported.[30][17][98][99] The prevalence of SS generally increases with age.[17]
Sjögren's syndrome is reported in 30-50% of people with rheumatoid arthritis and in 10-25% with systemic lupus erythematosus.[30]
History[edit]
Overview[edit]
The disease was described in 1933 by Henrik Sjögren, after whom it is named, but a number of earlier descriptions of people with the symptoms exist.[3]
History[edit]
Jan Mikulicz-Radecki (1850–1905) is generally credited with the first description of SS. In 1892, he described a 42-year-old man with enlargement of the parotid and lacrimal glands associated with a round-cell infiltrate and acinar atrophy.[52][100] However, the criteria that Mikulicz established for diagnosis often led to misdiagnosis of Mikulicz's syndrome. Many conditions, such as tuberculosis, infections, sarcoidosis and lymphoma present with similar conditions to those ascribed to Mikulicz's syndrome.[52] Nevertheless, the term "Mikulicz's syndrome" is still used occasionally to describe the appearance of lymphocytic infiltrates on salivary-gland biopsies.[52]
In 1930, Henrik Sjögren (1899–1986), an ophthalmologist in Jönköping, Sweden, observed a patient with low secretions from the lacrimal and salivary glands.[101] Sjögren introduced the term keratoconjunctivitis sicca for the symptom of dry eyes (keratoconjunctivitis). In 1933, he published his doctoral thesis describing 19 females, most of whom were postmenopausal and had arthritis, showing clinical and pathological manifestations of the syndrome.[100] Sjögren clarified that keratoconjunctivitis sicca, resulting from water deficiency, had no relation to xerophthalmia, resulting from vitamin A deficiency.[100] Sjögren's thesis was not well received as the Board of Examiners criticized some clinical aspects.[101]
After extensive research and data collection, Sjögren published an essential paper in 1951, describing 80 patients with keratoconjunctivitis sicca, 50 of whom also had arthritis.[101] His subsequent follow-up conference trips pertaining to his paper led to an international interest in Sjögren's syndrome.[101] The term "keratoconjunctivitis sicca" was coined by Sjögren himself and began to be identified as Sjögren's syndrome in literature,[101] although it can now have more general usage.