Threshold potential
In electrophysiology, the threshold potential is the critical level to which a membrane potential must be depolarized to initiate an action potential. In neuroscience, threshold potentials are necessary to regulate and propagate signaling in both the central nervous system (CNS) and the peripheral nervous system (PNS).
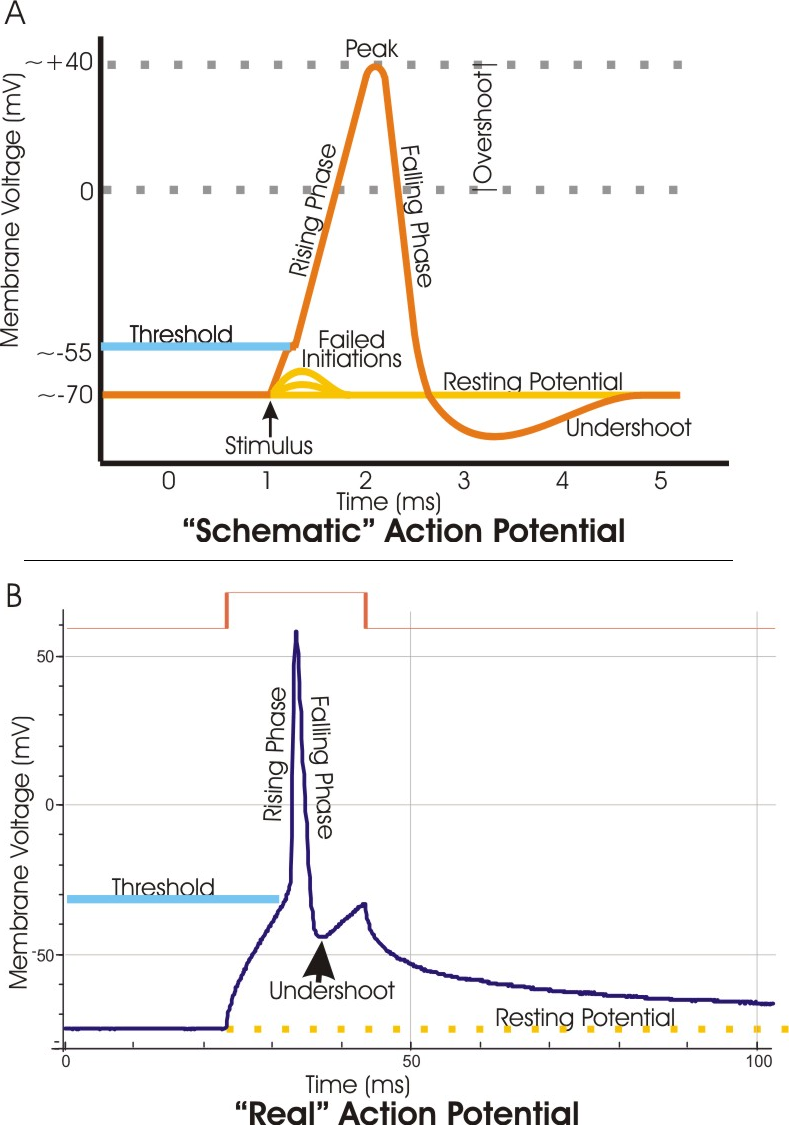
Most often, the threshold potential is a membrane potential value between –50 and –55 mV,[1] but can vary based upon several factors. A neuron's resting membrane potential (–70 mV) can be altered to either increase or decrease likelihood of reaching threshold via sodium and potassium ions. An influx of sodium into the cell through open, voltage-gated sodium channels can depolarize the membrane past threshold and thus excite it while an efflux of potassium or influx of chloride can hyperpolarize the cell and thus inhibit threshold from being reached.
Discovery[edit]
Initial experiments revolved around the concept that any electrical change that is brought about in neurons must occur through the action of ions. The German physical chemist Walther Nernst applied this concept in experiments to discover nervous excitability, and concluded that the local excitatory process through a semi-permeable membrane depends upon the ionic concentration. Also, ion concentration was shown to be the limiting factor in excitation. If the proper concentration of ions was attained, excitation would certainly occur.[2] This was the basis for discovering the threshold value.
Along with reconstructing the action potential in the 1950s, Alan Lloyd Hodgkin and Andrew Huxley were also able to experimentally determine the mechanism behind the threshold for excitation. It is known as the Hodgkin–Huxley model. Through use of voltage clamp techniques on a squid giant axon, they discovered that excitable tissues generally exhibit the phenomenon that a certain membrane potential must be reached in order to fire an action potential. Since the experiment yielded results through the observation of ionic conductance changes, Hodgkin and Huxley used these terms to discuss the threshold potential. They initially suggested that there must be a discontinuity in the conductance of either sodium or potassium, but in reality both conductances tended to vary smoothly along with the membrane potential.[3]
They soon discovered that at threshold potential, the inward and outward currents, of sodium and potassium ions respectively, were exactly equal and opposite. As opposed to the resting membrane potential, the threshold potential's conditions exhibited a balance of currents that were unstable. Instability refers to the fact that any further depolarization activates even more voltage-gated sodium channels, and the incoming sodium depolarizing current overcomes the delayed outward current of potassium.[4] At resting level, on the other hand, the potassium and sodium currents are equal and opposite in a stable manner, where a sudden, continuous flow of ions should not result. The basis is that at a certain level of depolarization, when the currents are equal and opposite in an unstable manner, any further entry of positive charge generates an action potential. This specific value of depolarization (in mV) is otherwise known as the threshold potential.