Transcranial magnetic stimulation
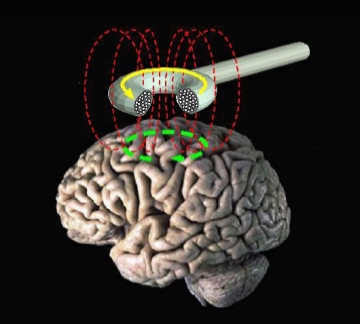
Transcranial magnetic stimulation (TMS) is a noninvasive form of brain stimulation in which a changing magnetic field is used to induce an electric current at a specific area of the brain through electromagnetic induction. An electric pulse generator, or stimulator, is connected to a magnetic coil connected to the scalp. The stimulator generates a changing electric current within the coil which creates a varying magnetic field, inducing a current within a region in the brain itself.[1]: 3 [2]
Transcranial magnetic stimulation
TMS has shown diagnostic and therapeutic potential in the central nervous system with a wide variety of disease states in neurology and mental health, with research still evolving.[3][4][5][6][7][8][9][10][11]
Adverse effects of TMS appear rare and include fainting and seizure.[12] Other potential issues include discomfort, pain, hypomania, cognitive change, hearing loss, and inadvertent current induction in implanted devices such as pacemakers or defibrillators.[12]
Adverse effects[edit]
Although TMS is generally regarded as safe, risks are increased for therapeutic rTMS compared to single or paired diagnostic TMS.[22] Adverse effects generally increase with higher frequency stimulation.[12]
The greatest immediate risk from TMS is fainting, though this is uncommon. Seizures have been reported, but are rare.[12][23][24] Other adverse effects include short term discomfort, pain, brief episodes of hypomania, cognitive change, hearing loss, impaired working memory, and the induction of electrical currents in implanted devices such as cardiac pacemakers.[12]
Procedure[edit]
During the procedure, a magnetic coil is positioned at the head of the person receiving the treatment using anatomical landmarks on the skull, in particular the inion and nasion.[13] The coil is then connected to a pulse generator, or stimulator, that delivers electric current to the coil.[2]
History[edit]
Luigi Galvani (1737–1798) undertook research on the effects of electricity on the body in the late-eighteenth century and laid the foundations for the field of electrophysiology.[38] In the 1830s Michael Faraday (1791–1867) discovered that an electrical current had a corresponding magnetic field, and that changing one could induce its counterpart.[39]
Work to directly stimulate the human brain with electricity started in the late 1800s, and by the 1930s the Italian physicians Cerletti and Bini had developed electroconvulsive therapy (ECT).[38] ECT became widely used to treat mental illness, and ultimately overused, as it began to be seen as a panacea. This led to a backlash in the 1970s.[38]
In 1980 Merton and Morton successfully used transcranial electrical stimulation (TES) to stimulate the motor cortex. However, this process was very uncomfortable, and subsequently Anthony T. Barker began to search for an alternative to TES.[40] He began exploring the use of magnetic fields to alter electrical signaling within the brain, and the first stable TMS devices were developed in 1985.[38][39] They were originally intended as diagnostic and research devices, with evaluation of their therapeutic potential being a later development.[38][39] The United States' FDA first approved TMS devices in October 2008.[38]