Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation.[8] GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea or shortness of breath, cough, sputum production and/or exacerbations) due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.[9]
Chronic obstructive pulmonary disease
Chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD)
Shortness of breath, chronic cough[1]
Over 35 years old[1]
Long term[1]
Stopping smoking, improving indoor and outdoor air quality, tobacco control measures[3][6]
174.5 million (2015)[7]
3.2 million (2019)[3]
The main symptoms of COPD include shortness of breath and a cough, which may or may not produce mucus.[4] COPD progressively worsens, with everyday activities such as walking or dressing becoming difficult.[3] While COPD is incurable, it is preventable and treatable. The two most common types of COPD are emphysema and chronic bronchitis and have been the two classic COPD phenotypes. However, this basic dogma has been challenged as varying degrees of co-existing emphysema, chronic bronchitis, and potentially significant vascular diseases have all been acknowledged in those with COPD, giving rise to the classification of other phenotypes or subtypes.[10]
Emphysema is defined as enlarged airspaces (alveoli) whose walls have broken down resulting in permanent damage to the lung tissue. Chronic bronchitis is defined as a productive cough that is present for at least three months each year for two years. Both of these conditions can exist without airflow limitation when they are not classed as COPD. Emphysema is just one of the structural abnormalities that can limit airflow and can exist without airflow limitation in a significant number of people.[11][12] Chronic bronchitis does not always result in airflow limitation. However, in young adults with chronic bronchitis who smoke, the risk of developing COPD is high.[13] Many definitions of COPD in the past included emphysema and chronic bronchitis, but these have never been included in GOLD report definitions.[8] Emphysema and chronic bronchitis remain the predominant phenotypes of COPD but there is often overlap between them and a number of other phenotypes have also been described.[10][14] COPD and asthma may coexist and converge in some individuals.[15] COPD is associated with low-grade systemic inflammation.[16]
The most common cause of COPD is tobacco smoking.[17] Other risk factors include indoor and outdoor air pollution including dust, exposure to occupational irritants such as dust from grains, cadmium dust or fumes, and genetics, such as alpha-1 antitrypsin deficiency.[13][18] In developing countries, common sources of household air pollution are the use of coal and biomass such as wood and dry dung as fuel for cooking and heating.[19][13] The diagnosis is based on poor airflow as measured by spirometry.[4]
Most cases of COPD can be prevented by reducing exposure to risk factors such as smoking and indoor and outdoor pollutants.[20] While treatment can slow worsening, there is no conclusive evidence that any medications can change the long-term decline in lung function.[6] COPD treatments include smoking cessation, vaccinations, pulmonary rehabilitation, inhaled bronchodilators and corticosteroids.[6] Some people may benefit from long-term oxygen therapy, lung volume reduction and lung transplantation.[21] In those who have periods of acute worsening, increased use of medications, antibiotics, corticosteroids and hospitalization may be needed.[22]
As of 2015, COPD affected about 174.5 million people (2.4% of the global population).[7] It typically occurs in males and females over the age of 35–40.[1][3] In 2019 it caused 3.2 million deaths, 80% occurring in lower and middle income countries,[3] up from 2.4 million deaths in 1990.[23][24] The number of deaths is projected to increase further because of continued exposure to risk factors and an aging population.[8] In the United States in 2010 the economic cost was put at US$32.1 billion and projected to rise to US$49 billion in 2020.[25] In the United Kingdom this cost is estimated at £3.8 billion annually.[26]
Exacerbations[edit]
An acute exacerbation is a sudden worsening of signs and symptoms that lasts for several days. The key symptom is increased breathlessness, other more pronounced symptoms are of excessive mucus, increased cough and wheeze. A commonly found sign is air trapping giving a difficulty in complete exhalation.[31]
The usual cause of an exacerbation is a viral infection, most often the common cold.[13] The common cold is usually associated with the winter months but can occur at any time.[32] Other respiratory infections may be bacterial or in combination sometimes secondary to a viral infection.[33] The most common bacterial infection is caused by Haemophilus influenzae.[34] Other risks include exposure to tobacco smoke (active and passive) and environmental pollutants – both indoor and outdoor.[35] During the COVID-19 pandemic, hospital admissions for COPD exacerbations sharply decreased which may be attributable to reduction of emissions and cleaner air.[36] There has also been a marked decrease in the number of cold and flu infections during this time.[37]
Smoke from wildfires is proving an increasing risk in many parts of the world and government agencies have published protective advice on their websites. In the US the EPA advises that the use of dust masks do not give protection from the fine particles in wildfires and instead advise the use of well-fitting particulate masks.[38] This same advice is offered in Canada and Australia to the effects of their forest fires.[39][40]
The number of exacerbations is not seen to relate to any stage of the disease; those with two or more a year are classed as frequent exacerbators and these lead to a worsening in the disease progression.[31] Frailty in ageing increases exacerbations and hospitalization.[41]
Acute exacerbations in COPD are often unexplained and thought to have many causes other than infections. A study has emphasized the possibility of a pulmonary embolism as sometimes being responsible in these cases. Signs can include pleuritic chest pain and heart failure without signs of infection. Such emboli could respond to anticoagulants.[42]
Subtypes[edit]
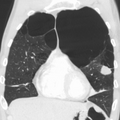
It has since been recognized that COPD is more complex, with a diverse group of disorders of differing risk factors and clinical courses that has resulted in a number of subtypes or phenotypes of COPD being accepted and proposed.[51][52] The two classic emphysematous and chronic bronchitic phenotypes are fundamentally different conditions with unique underlying mechanisms.[10] Another subtype of COPD, categorized by some as a separate clinical entity, is asthma-COPD overlap, which is a condition sharing clinical features of both asthma and COPD.[53][54] Spirometry measures are inadequate for defining phenotypes and chest X-ray, CT and MRI scans have been mostly employed. Most cases of COPD are diagnosed at a late stage and the use of imaging methods would allow earlier detection and treatment.[10]
The identification and recognition of different phenotypes can guide appropriate treatment approaches. For example, the PDE4 inhibitor roflumilast is targeted at the chronic-bronchitic phenotype.[55]
Two inflammatory phenotypes show a phenotype stability: the neutrophilic inflammatory phenotype and the eosinophilic inflammatory phenotype.[56] Mepolizumab, a monoclonal antibody, has been shown to have benefit in treating the eosinophilic inflammatory type rather than the use of oral corticosteroids, but further studies have been called for.[57]
Another recognized phenotype is the frequent exacerbator.[58] The frequent exacerbator has two or more exacerbations a year, has a poor prognosis and is described as a moderately stable phenotype.[31]
A pulmonary vascular COPD phenotype has been described due to cardiovascular dysfunction.[59] A molecular phenotype of CFTR dysfunction is shared with cystic fibrosis.[14] A combined phenotype of chronic bronchitis and bronchiectasis has been described with a difficulty noted of determining the best treatment.[60]
The only genotype is the alpha-1 antitrypsin deficiency (AATD) genetic subtype and this has a specific treatment.[61]
Epidemiology[edit]
Estimates of prevalence have considerable variation due to differences in analytical and surveying approach and the choice of diagnostic criteria.[208] An estimated 384 million people aged 30 years or more had COPD in 2010, corresponding to a global prevalence of 12%.[8] The disease affects men and women.[3] The increase in the developing world between 1970 and the 2000s is believed to be related to increasing rates of smoking in this region, an increasing population and an aging population due to fewer deaths from other causes such as infectious diseases.[136] Some developed countries have seen increased rates, some have remained stable and some have seen a decrease in COPD prevalence.[136]
Around three million people die of COPD each year.[8] In some countries, mortality has decreased in men but increased in women.[209] This is most likely due to rates of smoking in women and men becoming more similar.[88] A higher rate of COPD is found in those over 40 years and this increases greatly with advancing age with the highest rate found in those over 60 years.[8] Sex differences in the anatomy of the respiratory system include smaller airway lumens and thicker airway walls in women, which contribute to a greater severity of COPD symptoms like dyspnea and frequency of COPD exacerbation.[210]
In the UK, three million people are reported to be affected by COPD – two million of these being undiagnosed. On average, the number of COPD-related deaths between 2007 and 2016 was 28,600. The estimated number of deaths due to occupational exposure was estimated to be about 15% at around 4,000.[208] In the United States in 2018, almost 15.7 million people had been diagnosed with COPD and it is estimated that millions more have not been diagnosed.[211]
In 2011, there were approximately 730,000 hospitalizations in the United States for COPD.[212] Globally, COPD in 2019 was the third-leading cause of death. In low-income countries, COPD does not appear in the Top 10 causes of death; in other income groups, it is in the Top 5.[213]
Hyaluronan is a natural sugar in the extracellular matrix that provides a protective coating for cells. It has been shown that on exposure to pollution the hyaluronan in the lungs breaks down into fragments causing irritation and activation of the immune system. There follows subsequent airway constriction and inflammation. The study showed that the inhalation of unfragmented hyaluronan overcame the effects of fragmented HA and reduced inflammation. Inhaled HA only acts locally in the bronchial tree and does not interfere with any drug. It improves mucus clearance by allowing it to move more freely. Further studies are to be carried out in the
US to determine optimum dosage levels.[222]
A new cryogenic treatment aimed at the chronic bronchitic subtype using a liquid nitrogen metered cryospray is being trialled and was due to complete in September 2021.[223][224]
Stem-cell therapy using mesenchymal stem cells has the potential to restore lung function and thereby improve quality of life. In June 2021 eight clinical trials had been completed and seventeen were underway. Overall, stem cell therapy has proved to be safe. The trials include the use of stem cells from different sources such as adipose tissue, bone marrow and umbilical cord blood.[225]
A procedure known as targeted lung denervation is being trialled and has been used as part of a clinical trial (2021) in a hospital in the UK. The new minimally invasive procedure which takes about an hour to carry out, places electrodes to destroy branches of the vagus nerve in the lungs. The vagus nerve is responsible for both muscle contraction and mucus secretion, which results in narrowing the airways. In those with COPD these nerves are overactive, usually as a result of smoking damage and the constant mucus secretion and airway constriction leads to the symptoms of cough, shortness of breath, wheeze and tightness of the chest.[226]
The effectiveness of alpha-1 antitrypsin augmentation treatment for people who have alpha-1 antitrypsin deficiency is unclear.[227] A later clinical trial of double-dosing has shown some improvements in slowing the breakdown of elastin and the progression of emphysema with further studies being called for.[228]
Mass spectrometry is being studied as a diagnostic tool in COPD.[229]
Research continues into the use of telehealthcare to treat people with COPD when they experience episodes of shortness of breath; treating people remotely may reduce the number of emergency-room visits and improve the person's quality of life.[230]
Evidence is growing for the effectiveness of Astaxanthin against lung disease including COPD. Astaxanthin is a potent antioxidant with anti-inflammatory properties and more trials are said to be needed into its use.[231]
American COPD patients and their caregivers consider the following COPD-related research areas as the most important:
Other animals[edit]
Chronic obstructive pulmonary disease may occur in a number of other animals and may be caused by exposure to tobacco smoke.[233] Most cases of the disease, however, are relatively mild.[234] In horses it is known as recurrent airway obstruction (RAO) or heaves. RAO can be quite severe and most often is linked to exposure to common allergens.[235] COPD is also commonly found in old dogs.[236]