Addiction
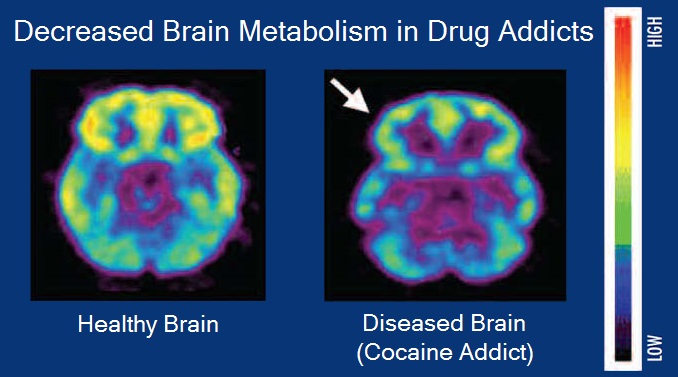
Addiction is a neuropsychological disorder characterized by a persistent and intense urge to use a drug or engage in a behaviour that produces natural reward, despite substantial harm and other negative consequences. Repetitive drug use often alters brain function in ways that perpetuate craving, and weakens (but does not completely negate) self-control.[1] This phenomenon – drugs reshaping brain function – has led to an understanding of addiction as a brain disorder with a complex variety of psychosocial as well as neurobiological (and thus involuntary)[a] factors that are implicated in addiction's development.[2][3][4] Classic signs of addiction include compulsive engagement in rewarding stimuli, preoccupation with substances or behavior, and continued use despite negative consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward),[5][6] coupled with delayed deleterious effects (long-term costs).[3][7]
"Addictive" redirects here. For other uses, see Addiction (disambiguation) and Addictive (disambiguation).Addiction
Addictive behaviour (e.g. substance-use addiction, sexual addiction), dependence, addictive disorder, addiction disorder (e.g. severe substance-use disorder, gambling disorder)
Examples of drug (or more generally, substance) addictions include alcoholism, cannabis addiction, amphetamine addiction, cocaine addiction, nicotine addiction, opioid addiction, and eating or food addiction. Behavioral addictions may include gambling addiction, shopping addiction, stalking, internet addiction, social media addiction, obsessive–compulsive disorder, video game addiction and sexual addiction. The DSM-5 and ICD-10 only recognize gambling addictions as behavioral addictions, but the ICD-11 also recognizes gaming addictions.[8]
Definitions[edit]
"Addiction" and "addictive behaviour" are polysemes denoting a category of mental disorders, of neuropsychological symptoms, or of merely maladaptive/harmful habits and lifestyles.[9] A common use of "addiction" in medicine is for neuropsychological symptoms denoting pervasive/excessive and intense urges to engage in a category of behavioral compulsions or impulses towards sensory rewards (e.g. alcohol, betel quid, drugs, sex, gambling, video gaming).[10][11][12][13][14] Addictive disorders or addiction disorders are mental disorders involving high intensities of addictions (as neuropsychological symptoms) that induce functional disabilities (i.e. limit subjects' social/family and occupational activities); the two categories of such disorders are substance-use addictions and behavioral addictions.[15][9][13][14]
However, there is no agreement on the exact definition of addiction in medicine. Indeed, Volkow et al. (2016) report that the DSM-5 defines addictions as the most severe degree of the addictive disorders, due to pervasive/excessive substance-use or behavioural compulsions/impulses.[16] It is a definition that many scientific papers and reports use.[17][18][19]
"Dependence" is also a polyseme denoting either neuropsychological symptoms or mental disorders. In the DSM-5, dependences differ from addictions and can even normally happen without addictions;[20] besides, substance-use dependences are severe stages of substance-use addictions (i.e. mental disorders) involving withdrawal issues.[21] In the ICD-11, "substance-use dependence" is a synonym of "substance-use addiction" (i.e. neuropsychological symptoms) that can but do not necessarily involve withdrawal issues.[22]
Signs and symptoms of addiction can vary depending on the type of addiction. Symptoms of drug addictions may include:
Signs and symptoms of addiction may include:
Screening and assessment[edit]
Addictions Neuroclinical Assessment[edit]
The Addictions Neuroclinical Assessment is used to diagnose addiction disorders. This tool measures three different domains: executive function, incentive salience, and negative emotionality.[68][69] Executive functioning consists of processes that would be disrupted in addiction.[69] In the context of addiction, incentive salience determines how one perceives the addictive substance.[69] Increased negative emotional responses have been found with individuals with addictions.[69]
Tobacco, Alcohol, Prescription Medication, and Other Substance Use (TAPS)[edit]
This is a screening and assessment tool in one, assessing commonly used substances. This tool allows for a simple diagnosis, eliminating the need for several screening and assessment tools, as it includes both TAPS-1 and TAPS-2, screening and assessment tools respectively. The screening component asks about the frequency of use of the specific substance (tobacco, alcohol, prescription medication, and other).[70] If an individual screens positive, the second component will begin. This dictates the risk level of the substance.[70]
CRAFFT[edit]
The CRAFFT (Car-Relax-Alone-Forget-Family and Friends-Trouble) is a screening tool that is used in medical centers. The CRAFFT is in version 2.1 and has a version for nicotine and tobacco use called the CRAFFT 2.1+N.[71] This tool is used to identify substance use, substance related driving risk, and addictions among adolescents. This tool uses a set of questions for different scenarios.[72] In the case of a specific combination of answers, different question sets can be used to yield a more accurate answer. After the questions, the DSM-5 criteria are used to identify the likelihood of the person having substance use disorder.[72] After these tests are done, the clinician is to give the "5 RS" of brief counseling.
The five Rs of brief counseling includes:
Social learning models[edit]
Social learning theory[edit]
Main article: Social learning theory
Albert Bandura's 1977 social learning theory posits that individuals acquire addictive behaviors by observing and imitating models in their social environment.[292][293] The likelihood of engaging in and sustaining similar addictive behaviors is influenced by the reinforcement and punishment observed in others. The principle of reciprocal determinism suggests that the functional relationships between personal, environmental, and behavioral factors act as determinants of addictive behavior.[294] Thus, effective treatment targets each dynamic facet of the biopsychosocial disorder.
Transtheoretical model (stages of change model)[edit]
Main article: Transtheoretical model
The transtheoretical model of change suggests that overcoming an addiction is a stepwise process that occurs through several stages.[295]
Precontemplation: This initial stage precedes individuals considering a change in their behavior. They might be oblivious to or in denial of their addiction, failing to recognize the need for change.
Contemplation is the stage in which individuals become aware of the problems caused by their addiction and are considering change. Although they may not fully commit, they weigh the costs and benefits of making a shift.
Preparation: Individuals in this stage are getting ready to change. They might have taken preliminary steps, like gathering information or making small commitments, in preparation for behavioral change.
Action involves actively modifying behavior by making specific, observable changes to address the addictive behavior. The action stage requires significant effort and commitment.
Maintenance: After successfully implementing a change, individuals enter the maintenance stage, where they work to sustain the new behavior and prevent relapse. This stage is characterized by ongoing effort and consolidation of gains.
Termination/relapse prevention: Recognizing that relapse is a common part of the change process, this stage focuses on identifying and addressing factors that may lead to a return to old behaviors. Relapse is viewed as an opportunity for learning and strategy adjustment, with the ultimate goal of completely eliminating or terminating the targeted behavior.
The transtheoretical model can be helpful in guiding development of tailored behavioral interventions that can promote lasting change. Progression through these stages may not always follow a linear path, as individuals may move back and forth between stages. Resistance to change is recognized as an expected part of the process.
Addiction causes an "astoundingly high financial and human toll" on individuals and society as a whole.[296][230][233] In the United States, the total economic cost to society is greater than that of all types of diabetes and all cancers combined.[233] These costs arise from the direct adverse effects of drugs and associated healthcare costs (e.g., emergency medical services and outpatient and inpatient care), long-term complications (e.g., lung cancer from smoking tobacco products, liver cirrhosis and dementia from chronic alcohol consumption, and meth mouth from methamphetamine use), the loss of productivity and associated welfare costs, fatal and non-fatal accidents (e.g., traffic collisions), suicides, homicides, and incarceration, among others.[296][230][233][297] The US National Institute on Drug Abuse has found that overdose deaths in the US have almost tripled among male and females from 2002 to 2017, with 72,306 overdose deaths reported in 2017 in the US.[298] 2020 marked the year with highest number of overdose deaths over a 12-month period, with 81,000 overdose deaths, exceeding the records set in 2017.[299]
Kyoto Encyclopedia of Genes and Genomes (KEGG) signal transduction pathways: