Opioid overdose
An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone.[3][5] This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia from slow and shallow breathing.[3] Other symptoms include small pupils[note 1] and unconsciousness; however, its onset can depend on the method of ingestion, the dosage and individual risk factors.[6] Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.[7][8]
Opioid overdose
Narcotic overdose, opioid poisoning
Opioid dependence, metabolic disorders, use of high doses of opioids, injection of opioids, use with antidepressants, alcohol, benzodiazepines and cocaine.[1][2]
Based on symptoms[3]
Improved access to naloxone, treatment of opioid dependence
Supporting a person's breathing and naloxone
over 110,000 (2017)
Opioid overdoses are diagnosed based on symptoms and examination.[3] Risk factors for opioid overdose include high levels of opioid dependence, use of opioids via injection, high dosed opioid usage, having a mental disorder or having a predisposition for one, and use of opioids in combination with other substances, such as alcohol, benzodiazepines, or cocaine.[1][9][2] Dependence on prescription opioids can occur from their use to treat chronic pain in individuals.[1] Additionally, if following a period of detoxification, which allows the tolerance level to fall, the risk of overdose upon return to use is high.[1]
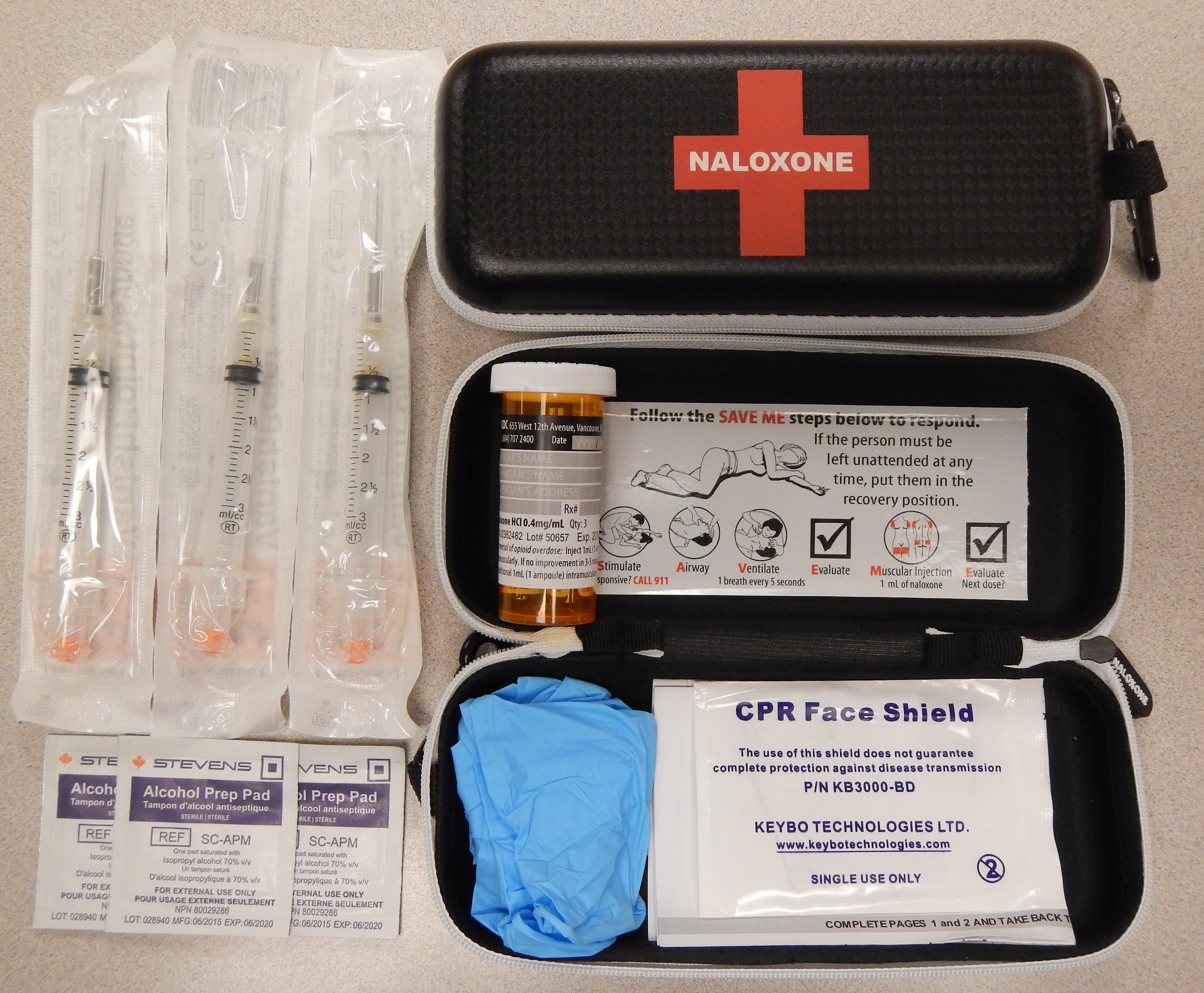
Initial treatment of an overdose involves supporting the person's breathing and providing oxygen to reduce the risk of hypoxia.[10] Naloxone is then recommended to those who cannot reverse the opioid's effects through breathing.[10][3] Giving naloxone via nasal administration or as an injection into a muscle has shown to be equally effective.[11] Other efforts to prevent deaths from overdose include increasing access to naloxone and treatment for opioid dependence.[1][12]
Drug use contributes to 500,000 deaths worldwide, with opioid overdose resulting in approximately 115,000 of these deaths in 2018.[1] This is up from 18,000 deaths in 1990.[13][14] In 2018, approximately 269 million people had engaged in drug usage at least once, 58 million of which used opioids.[1] Drug use disorders have affected around 35.6 million people worldwide in 2018.[1] The WHO estimates that 70% of deaths due to drug use are in relation to opioids, with 30% being due to overdose.[1] It is believed that the opioid epidemic has partly been caused due to assurances that prescription opioids were safe, by the pharmaceutical industry in the 1990s.[15] This led to unwarranted trust and a subsequent heavy reliance on opioids.[15] Though there are treatment interventions which can effectively reduce the risk of overdose in people with opioid dependence, less than 10% of affected individuals receive it.[1]
Prevention[edit]
Opioid overdoses can often be prevented.[35][36] Clear protocols for staff at emergency departments and urgent care centers can reduce opioid prescriptions for individuals presenting in these settings who engage in drug seeking behaviors or who have a history of substance abuse.[37] Drug seeking behaviors include but are not limited to obsessiveness or impatience when it comes to attaining medications, seeking multiple pain adjunct medications, and inconsistent physiological presentation.[38] A prescription monitoring program may help determine if an individual is receiving a high doses of opioids or combinations of medications such as benzodiazepines and opioids that put them at high risk.[39] Limited amount of evidence suggests opioid therapy with extended-release or long-acting formulations may increase the risk of an unintentional overdose compared to shorter-acting agents.[40] Routinely screening using tools such as the CAGE-AID and the Drug Abuse Screening Test (DAST-10) in adults and the CRAFFT in those aged 14–18 years is recommended.[35] The revised risk index for overdose or severe opioid induced respiratory depression (RIOSORD) is a validated screening tool that may be used to estimate the risk of overdose in people using opioids, or the rapid opioid dependence screen may be used as a more rapid and succinct method to screen for opioid use disorder.[24] Other "drug seeking" behaviors and physical indications of drug use should be used as clues to perform formal screenings.[35]
There are several medication-assisted treatments available for people with opioid use disorder or opioid dependence, who are at higher risk for opioid overdose.[1][41] The selection of treatment depends on various factors, such as a person's preference, accessibility, and history of treatment.[41] Examples of medication-assisted treatments are buprenorphine (with or without naloxone), naltrexone, and methadone.[42][43] Methadone and buprenorphine are associated with reduced mortality in those with opioid use disorder as well as higher drug treatment program retention, lower illicit drug use and decreased overdose deaths.[24] The mortality benefit of long term naltrexone use in those with opioid use disorder is less well established.[24] After a non-fatal opioid overdose, subsequent methadone or buprenorphine initiation and use reduce the risk of overdose death by 59% and 38% respectively. Initiating buprenorphine in the emergency department is associated with lower mortality and increased adherence to opioid use disorder treatment programs.[24] Peer support groups have tentative evidence of benefit.[44] There is also some evidence indicating benefits in community-based overdose education and naloxone distribution programs.[45] Buprenorphine and methadone can help decrease drug cravings.[41] Combining pharmacologic treatments with behavioral therapy, such as support or recovery groups, can increase likelihood of overcoming addiction and reduce the risk of an opioid overdose.
Individuals diagnosed with opioid dependence should be prescribed naloxone to prevent overdose and should be directed to one of treatment options available, such as needle exchange programs and treatment centers.[35][36] A naloxone prescription is also recommended when risk factors for opioid overdose are present such as history of overdose, substance use disorder, or higher doses of opioids.[39] With the CDC recommending naloxone be provided to all people on long term opioids who have risk factors for overdose, including a history of a substance use disorder, daily morphine equivalents greater than 50 mg or concurrent benzodiazepine use.[24] Brief motivational interviewing can also be performed and has been shown to improve people's motivation to change their behavior.[35][46] Despite these opportunities, the dissemination of prevention interventions in the US has been hampered by the lack of coordination and sluggish federal government response.[36]
Unused or old opioids should not be stored in the home as there is a risk of people using the drugs for non-medical purposes. Among adolescents and young-adults, non-medical use of prescription opioids is associated with a subsequent 13-fold increased risk of heroin use later in life.[24] Opioids that are no longer being used may be taken to drug take back programs at local pharmacies, healthcare facilities or law enforcement agencies for safe disposal. The United States Food and Drug Administration also has a "flush list"; a list of medications that may be safely disposed of by flushing down the toilet.[47]
In the United States, 49 states and the District of Columbia have expanded naloxone access at a pharmacy level via standing order, protocol order, naloxone-specific collaborative practice agreement, or pharmacist prescriptive authority.[48]
Awareness[edit]
The Substance Abuse and Mental Health Services Administration hosts an annual health observance known as National Prevention Week. Every third week of May, they encourage communities across the country to unite to share stories about positive mental and behavioral health and the importance of implementing prevention methods.[69] They also sponsor recovery Month every September. Recovery Month aims to raise awareness about mental and substance use disorders and to honor individuals who recover, promoting the positive message that prevention works and that treatment is effective.[70]
International Overdose Awareness Day is on 31 August to remember those who have died from an overdose, to decrease stigma of drug-related deaths, and to promote prevention of overdose.[71]
![US yearly deaths from all opioid drugs. Included in this number are opioid analgesics, along with heroin and illicit synthetic opioids.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/8/87/US_timeline._Opioid_deaths.jpg/360px-US_timeline._Opioid_deaths.jpg)
![US yearly deaths involving other synthetic opioids, predominately Fentanyl.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3e/US_timeline._Deaths_involving_other_synthetic_opioids%2C_predominately_Fentanyl.jpg/369px-US_timeline._Deaths_involving_other_synthetic_opioids%2C_predominately_Fentanyl.jpg)
![US yearly deaths involving prescription opioids. Non-methadone synthetics is a category dominated by illegally acquired fentanyl, and has been excluded.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/c/c1/US_timeline._Prescription_opioid_pain_reliever_deaths.jpg/360px-US_timeline._Prescription_opioid_pain_reliever_deaths.jpg)
![US yearly overdose deaths involving heroin.[2]](http://upload.wikimedia.org/wikipedia/commons/thumb/8/8d/Timeline_of_US_overdose_deaths_involving_heroin%2C_by_other_opioid_involvement.jpg/360px-Timeline_of_US_overdose_deaths_involving_heroin%2C_by_other_opioid_involvement.jpg)