Portal hypertension
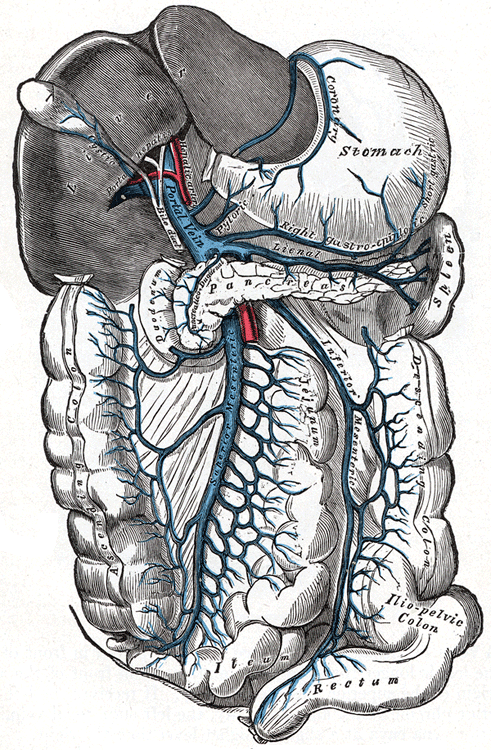
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg.[3][4] Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5–9 mmHg; clinically significant portal hypertension is present at portal pressures greater than 10 mmHg.[5] The portal vein and its branches supply most of the blood and nutrients from the intestine to the liver.[6]
Cirrhosis (a form of chronic liver failure) is the most common cause of portal hypertension; other, less frequent causes are therefore grouped as non-cirrhotic portal hypertension. The signs and symptoms of both cirrhotic and non-cirrhotic portal hypertension are often similar depending on cause, with patients presenting with abdominal swelling due to ascites, vomiting of blood, and lab abnormalities such as elevated liver enzymes or low platelet counts.
Treatment is directed towards decreasing portal hypertension itself or in the management of its acute and chronic complications.[7] Complications include ascites, spontaneous bacterial peritonitis, variceal hemorrhage, hepatic encephalopathy, hepatorenal syndrome, and cardiomyopathy.
Signs and symptoms of portal hypertension include:
In addition, a widened (dilated) portal vein as seen on a CT scan or MRI may raise the suspicion about portal hypertension. A cutoff value of 13 mm is widely used in this regard, but the diameter is often larger than this is in normal individuals as well.[9]
The causes for portal hypertension are classified as originating in the portal venous system before it reaches the liver (prehepatic causes), within the liver (intrahepatic) or between the liver and the heart (post-hepatic). The most common cause is cirrhosis (chronic liver failure). Other causes include:[1][10][11]
Prehepatic causes
Hepatic causes
Posthepatic causes