Temporomandibular joint dysfunction
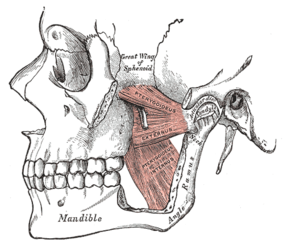
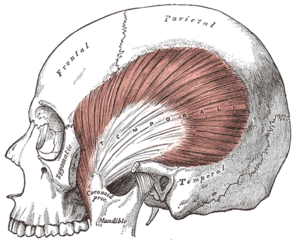
Temporomandibular joint dysfunction (TMD, TMJD) is an umbrella term covering pain and dysfunction of the muscles of mastication (the muscles that move the jaw) and the temporomandibular joints (the joints which connect the mandible to the skull). The most important feature is pain, followed by restricted mandibular movement,[2] and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to quality of life;[3] this is because the symptoms can become chronic and difficult to manage.
This article is about the syndrome with joint pain. For the range of diseases affecting the joint, see Temporomandibular joint pathology.Temporomandibular joint dysfunction
Temporomandibular joint dysfunction syndrome, temporomandibular disorder, others[1]
In this article, the term temporomandibular disorder is taken to mean any disorder that affects the temporomandibular joint, and temporomandibular joint dysfunction (here also abbreviated to TMD) is taken to mean symptomatic (e.g. pain, limitation of movement, clicking) dysfunction of the temporomandibular joint. However, there is no single, globally accepted term or definition[4] concerning this topic.
TMDs have a range of causes and often co-occur with a number of overlapping medical conditions, including headaches, fibromyalgia, back pain, and irritable bowel.[5] However, these factors are poorly understood,[6] and there is disagreement as to their relative importance. There are many treatments available,[7] although there is a general lack of evidence for any treatment in TMD, and no widely accepted treatment protocol. Common treatments include provision of occlusal splints, psychosocial interventions like cognitive behavioral therapy, physical therapy, and pain medication or others. Most sources agree that no irreversible treatment should be carried out for TMD.[8]
About 20% to 30% of the adult population are affected to some degree.[7] Usually people affected by TMD are between 20 and 40 years of age,[3] and it is more common in females than males.[9] TMD is the second most frequent cause of orofacial pain after dental pain (i.e. toothache).[10]
Signs and symptoms of temporomandibular joint disorder vary in their presentation. The symptoms will usually involve more than one of the various components of the masticatory system, muscles, nerves, tendons, ligaments, bones, connective tissue, or the teeth.[22]
The three classically described, cardinal signs and symptoms of TMD are:[10][23]
TMJ dysfunction is commonly associated with symptoms affecting cervical spine dysfunction and altered head and cervical spine posture.[25]
Other signs and symptoms have also been described, although these are less common and less significant than the cardinal signs and symptoms listed above. Examples include:
Prognosis[edit]
It has been suggested that the natural history of TMD is benign and self-limiting,[24] with symptoms slowly improving and resolving over time.[14] The prognosis is therefore good.[4] However, the persistent pain symptoms, psychological discomfort, physical disability and functional limitations may detriment quality of life.[91] It has been suggested that TMD does not cause permanent damage and does not progress to arthritis in later life,[24]: 174–175 however, degenerative disorders of the TMJ such as osteoarthritis are included within the spectrum of TMDs in some classifications.
Epidemiology[edit]
TMD mostly affects people in the 20 – 40 age group,[7] and the average age is 33.9 years.[9] People with TMD tend to be younger adults,[4] who are otherwise healthy. Within the catchall umbrella of TMD, there are peaks for disc displacements at age 30, and for inflammatory-degenerative joint disorders at age 50.[10]
About 75% of the general population may have at least one abnormal sign associated with the TMJ (e.g. clicking), and about 33% have at least one symptom of TMD.[23] However, only in 3.6–7% will this be of sufficient severity to trigger the individual to seek medical advice.[23]
For unknown reasons, females are more likely to be affected than males, in a ratio of about 2:1,[9] although others report this ratio to be as high as 9:1.[23] Females are more likely to request treatment for TMD, and their symptoms are less likely to resolve.[23] Females with TMD are more likely to be nulliparous than females without TMD.[26] It has also been reported that female caucasians are more likely to be affected by TMD, and at an earlier age, than female African Americans.[4]
According to the most recent analyses of epidemiologic data using the RDC/TMD diagnostic criteria, of all TMD cases, group I (muscle disorders) accounts for 45.3%, group II (disc displacements) 41.1%, and group III (joint disorders) 30.1% (individuals may have diagnoses from more than one group).[10] Using the RDC/TMD criteria, TMD has a prevalence in the general population of 9.7% for group I, 11.4% for group IIa, and 2.6% for group IIIa.[10]
History[edit]
Temporomandibular disorders were described as early as ancient Egypt.[23] An older name for the condition is "Costen's syndrome", eponymously referring to James B. Costen.[92][93] Costen was an otolaryngologist,[94] and although he was not the first physician to describe TMD, he wrote extensively on the topic, starting in 1934, and was the first to approach the disorder in an integrated and systematic way.[95] Costen hypothesized that malocclusion caused TMD, and placed emphasis on ear symptoms, such as tinnitus, otalgia, impaired hearing, and even dizziness.[95] Specifically, Costen believed that the cause of TMD was mandibular over-closure,[94] recommending a treatment revolving around building up the bite.[94] The eponym "Costen syndrome" became commonly used shortly after his initial work,[95] but in modern times it has been dropped, partially because occlusal factors are now thought to play little, if any, role in the development of TMD,[4] and also because ear problems are now thought to be less associated with TMD. Other historically important terms that were used for TMD include "TMJ disease" or "TMJ syndrome", which are now rarely used.[4]