Toxoplasma gondii
Toxoplasma gondii (/ˈtɒksəˌplæzmə ˈɡɒndi.aɪ, -iː/) is a parasitic protozoan (specifically an apicomplexan) that causes toxoplasmosis.[3] Found worldwide, T. gondii is capable of infecting virtually all warm-blooded animals,[4]: 1 but felids are the only known definitive hosts in which the parasite may undergo sexual reproduction.[5][6]
In rodents, T. gondii alters behavior in ways that increase the rodents' chances of being preyed upon by felids.[7][8][9] Support for this "manipulation hypothesis" stems from studies showing that T. gondii-infected rats have a decreased aversion to cat urine while infection in mice lowers general anxiety, increases explorative behaviors and increases a loss of aversion to predators in general.[7][10] Because cats are one of the only hosts within which T. gondii can sexually reproduce, such behavioral manipulations are thought to be evolutionary adaptations that increase the parasite's reproductive success since rodents that do not avoid cat habitations will more likely become cat prey.[7] The primary mechanisms of T. gondii–induced behavioral changes in rodents occur through epigenetic remodeling in neurons that govern the relevant behaviors (e.g. hypomethylation of arginine vasopressin-related genes in the medial amygdala, which greatly decrease predator aversion).[11][12]
In humans, particularly infants and those with weakened immunity, T. gondii infection is generally asymptomatic but may lead to a serious case of toxoplasmosis.[13][4] T. gondii can initially cause mild, flu-like symptoms in the first few weeks following exposure, but otherwise, healthy human adults are asymptomatic.[14][13][4] This asymptomatic state of infection is referred to as a latent infection, and it has been associated with numerous subtle behavioral, psychiatric, and personality alterations in humans.[14][15][16] Behavioral changes observed between infected and non-infected humans include a decreased aversion to cat urine (but with divergent trajectories by gender) and an increased risk of several psychiatric disorders – particularly schizophrenia and bipolar disorder.[17] Preliminary evidence has suggested that T. gondii infection may induce some of the same alterations in the human brain as those observed in rodents.[18][19][9][20][21][22] Many of these associations have been strongly debated and newer studies have found them to be weak, concluding:[23]
T. gondii is one of the most common parasites in developed countries;[24][25] serological studies estimate that up to 50% of the global population has been exposed to, and may be chronically infected with, T. gondii; although infection rates differ significantly from country to country.[14][26] Estimates have shown the highest IgG seroprevalence to be in Ethiopia, at 64.2%, as of 2018.[27]
The following have been identified as being risk factors for T. gondii infection in humans and warm-blooded animals:
A common argument in the debate about whether cat ownership is ethical involves the question of Toxoplasma gondii transmission to humans.[60] Even though "living in a household with a cat that used a litter box was strongly associated with infection,"[31] and that living with several kittens or any cat under one year of age has some significance,[50] several other studies claim to have shown that living in a household with a cat is not a significant risk factor for T. gondii infection.[51][61]
Specific vectors for transmission may also differ based on geographic location. "The seawater in California is thought to be contaminated by T. gondii oocysts that originate from cat feces, survive or bypass sewage treatment, and travel to the coast through river systems. T. gondii has been identified in a California mussel by polymerase chain reaction and DNA sequencing. In light of the potential presence of T. gondii, pregnant women and immunosuppressed persons should be aware of this potential risk associated with eating raw oysters, mussels, and clams."[50]
In warm-blooded animals, such as brown rats, sheep, and dogs, T. gondii has also been shown to be sexually transmitted.[62][63][64] Although T. gondii can infect, be transmitted by, and asexually reproduce within humans and virtually all other warm-blooded animals, the parasite can sexually reproduce only within the intestines of members of the cat family (felids).[30] Felids are therefore the definitive hosts of T. gondii; all other hosts (such as human or other mammals) are intermediate hosts.
Treatment[edit]
In humans, active toxoplasmosis can be treated with a combination of drugs such as pyrimethamine and sulfadiazine, plus folinic acid. Immune-compromised patients may need continuous treatment until/unless their immune system is restored.[71]
Water transmission[edit]
The transmission of oocysts has been unknown, even though there have many documented cases of infection in marine species. Researchers have found that the oocytes of T. gondii can survive in seawater for at least 6 months, with the amount of salt concentration not affecting its life cycle. There have been no studies on the ability of T. gondii oocysts life cycle within freshwater environments, although infections are still present. One possible hypothesis of transmission is via amoeba species, particularly Acanthamoeba spp., a species that is found in all water environments (fresh, brackish, and full-strength seawater). Normally, amoebas function as a natural filter, phagocytizing nutrients and bacteria found within the water. Some pathogens have used this to their advantage, however, and evolved to be able to avoid being broken down and, thus, survive encased in the amoeba – this includes Holosporaceae, Pseudomonaceae, Burkholderiacceae, among others.[78] Overall, this aids the pathogen in transportation but, also, protection from drugs and sterilizers that would, otherwise, cause death in the pathogen.[79] Studies have shown that T. gondii oocysts can live within amoebas after being engulfed for at least 14 days without significant obliteration of the parasite.[80] The ability of the microorganism to survive in vitro is dependent on the microorganism itself, but there are a few overarching mechanisms present. T. gondii oocysts have been found to resist an acidic pH and, thus, are protected by the acidification found in endocytic vacuoles and lysosomes.[80] Phagocytosis further increases with the carbohydrate-rich surface membrane located on the amoebae.[81] The pathogen can be released either by lysis of the amoebae or by exocytosis, but this is understudied [82]
Impact on wild birds[edit]
Almost all species of birds that have been tested for Toxoplasma gondii have shown to be positive. The only bird species not reported with clinical symptoms of toxoplasmosis would be wild ducks, and there has only been one report found on domesticated ducks occurring in 1962.[83] Species with resistance toward T. gondii include domestic turkeys,[84] owls, red tail hawks, and sparrows, depending on the strain of T. gondii.[85] T. gondii is considerably more severe in pigeons, particularly crown pigeons, ornamental pigeons, and pigeons originating from Australia and New Zealand. Typical onset is quick and usually results in death. Those that do survive often have chronic conditions of encephalitis and neuritis.[85] Similarly, canaries are observed to be just as severe as pigeons, but the clinical symptoms are more abnormal when compared to other species. Most of the infection affects the eye, causing blindness, choroidal lesions, conjunctivitis, atrophy of the eye, blepharitis, and chorioretinitis [85] Most of the time, the infection leads to death.
Current environmental efforts[edit]
Urbanization and global warming are extremely influential in the transmission of T. gondii.[86] Temperature and humidity are huge factors in the sporulation stage: low humidity is always fatal to the oocysts, and they are also vulnerable to extreme temperatures.[86] Rainfall is also an important factor for survival of waterborne pathogens. Because increased rainfall directly increases the flow rate in rivers, the amount of flow into coastal areas is increased as well. This can spread waterborne pathogens over wide areas.
There is no effective vaccine for T. gondii, and research on a live vaccine is ongoing. Feeding cats commercially available food, rather than raw, undercooked meat, prevents felines from becoming a host for oocysts, as higher prevalence is in areas where raw meat is fed.[87] Researchers also suggest that owners restrict cats to live indoors and to be neutered or spayed to decrease stray cat populations and to reduce intermediate host interactions. It is suggested that fecal matter from litter boxes be collected daily, placed in a sealable bag, and disposed of in the trash rather than flushed in the toilet, so that water contamination is limited.[88]
Studies have found that wetlands with a high density of vegetation decrease the concentration of oocysts in water through two possible mechanisms. Firstly, vegetation decreases flow velocities, which enables more settling because of increased transport time.[88] Secondly, the vegetation can remove oocysts through its ability to mechanically strain the water, as well as through the process of adhesion (i.e. attachment to biofilms). Areas of erosion and destruction of coastal wetlands have been found to harbour increased concentrations of T. gondii oocysts, which then flow into open coastal waters. Current physical and chemical treatments typically utilized in water treatment facilities have been proven to be ineffective against T. gondii. Research has shown that UV-C disinfection of water containing oocysts results in inactivation and possible sterilization.[89]
Genome[edit]
The genomes of more than 60 strains of T. gondii have been sequenced. Most are 60–80 Mb in size and consist of 11–14 chromosomes.[90][91] The major strains encode 7,800–10,000 proteins, of which about 5,200 are conserved across RH, GT1, ME49, VEG.[90] A database, ToxoDB, has been established to document genomic information on Toxoplasma.[92][93][94]
History[edit]
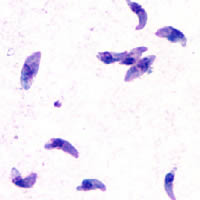
In 1908, while working at the Pasteur Institute in Tunis, Charles Nicolle and Louis Manceaux discovered a protozoan organism in the tissues of a hamster-like rodent known as the gundi, Ctenodactylus gundi.[30] Although Nicolle and Manceaux initially believed the organism to be a member of the genus Leishmania that they described as "Leishmania gondii", they soon realized they had discovered a new organism entirely; they renamed it Toxoplasma gondii. The new genus name Toxoplasma is a reference to its morphology: Toxo, from Greek τόξον (toxon, 'arc, bow'), and πλάσμα (plasma, 'shape, form') and the host in which it was discovered, the gundi (gondii).[95] The same year Nicolle and Mancaeux discovered T. gondii, Alfonso Splendore identified the same organism in a rabbit in Brazil. However, he did not give it a name.[30] In 1914, Italian tropicalist Aldo Castellani "was first to suspect that toxoplasmosis could affect humans".[96]
The first conclusive identification of T. gondii in humans was in an infant girl delivered full term by Caesarean section on May 23, 1938, at Babies' Hospital in New York City.[30] The girl began having seizures at three days of age, and doctors identified lesions in the maculae of both of her eyes. When she died at one month of age, an autopsy was performed. Lesions discovered in her brain and eye tissue were found to have both free and intracellular T. gondii'.[30] Infected tissue from the girl was homogenized and inoculated intracerebrally into rabbits and mice; they then developed encephalitis. Later, congenital transmission was confirmed in many other species, particularly infected sheep and rodents.
The possibility of T. gondii transmission via consumption of undercooked meat was first proposed by D. Weinman and A.H Chandler in 1954.[30] In 1960, the relevant cyst wall were shown to dissolve in the proteolytic enzymes found in the stomach, releasing infectious bradyzoites into the stomach (which pass into the intestine). The hypothesis of transmission via consumption of undercooked meat was tested in an orphanage in Paris in 1965; incidence of T. gondii rose from 10% to 50% after a year of adding two portions of cooked-rare beef or horse meat to many orphans' daily diets, and to 100% among those fed cooked-rare lamb chops.[30]
A 1959 Mumbai-based study found there prevalence in strict vegetarians was similar to that of non-vegetarians. This raised the possibility of a third major route of infection, beyond congenital and non well-cooked meat carnivorous transmission.[30]
In 1970, oocysts were found in (cat) feces. The fecal–oral route of infection via oocysts was demonstrated.[30] In the 1970s and 1980s feces of a vast range of infected animal species was tested to see if it contained oocysts — at least 17 species of felids shed oocysts, but no non-felid has been shown to allow T. gondii sexual reproduction (leading to oocyst shedding).[30]
In 1984 Elmer R. Pfefferkorn published his discovery that treatment of human fibroblasts with human recombinant interferon gamma blocks the growth of T. gondii.[97]
There are many instances where behavioural changes were reported in rodents with T. gondii. The changes seen were a reduction in their innate dislike of cats, which made it easier for cats to prey on the rodents. In an experiment conducted by Berdoy and colleagues, the infected rats showed preference for the cat odour area versus the area with the rabbit scent, therefore making it easier for the parasite to take its final step in its definitive feline host.[7] This is an example of the extended phenotype concept, that is, the idea that the behaviour of the infected animal changes in order to maximize survival of the genes that increase predation of the intermediate rodent host.[98]
As mentioned before, these results of increased proportions of people seropositive for the parasite in cases of these neurological disorders do not necessarily indicate a causal relationship between the infection and disorder. It is also important to mention that in 2016 a population-representative birth cohort study which was done, to test a hypothesis that toxoplasmosis is related to impairment in brain and behaviour measured by a range of phenotypes including neuropsychiatric disorders, poor impulse control, personality and neurocognitive deficits. The results of this study did not support the results in the previously mentioned studies, more than marginally. None of the P-values showed significance for any outcome measure. Thus, according to this study, the presence of T. gondii antibodies is not correlated to increase susceptibility to any of the behaviour phenotypes (except possibly to a higher rate of unsuccessful attempted suicide). This team did not observe any significant association between T. gondii seropositivity and schizophrenia. The team notes that the null findings might be a false negative due to low statistical power because of small sample sizes but against this weights that their setup should avoid some possibilities for errors in the about 40 studies that did show a positive correlation. They concluded that further studies should be performed.[113]
The mechanism behind behavioral changes is partially attributed to increased dopamine metabolism,[114] which can be neutralized by dopamine antagonist medications.[115] T. gondii has two genes that code for a bifunctional phenylalanine and tyrosine hydroxylase, two important and rate-limiting steps of dopamine biosynthesis. One of the genes is constitutively expressed, while the other is only produced during cyst development.[116][117] In addition to additional dopamine production, T. gondii infection also produces long-lasting epigenetic changes in animals that increase the expression of vasopressin, a probable cause of alterations that persist after the clearance of the infection.[118]
In 2022, a study published in Communications Biology of a well-documented population of wolves studied throughout their lives, suggested that T. gondii also may have a significant effect on their behavior.[119] It suggested that infection with this parasite emboldened infected wolves into behavior that determined leadership roles and influenced risk-taking behavior, perhaps even motivating establishment of new independent packs that they would establish and lead in behavior patterns differing from that of the packs into which they were born. The study determined that at times, an infected wolf would become the only breeding male in a pack, leading to a significant effect on another species by T. gondii.