Traumatic brain injury
A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity ranging from mild traumatic brain injury (mTBI/concussion) to severe traumatic brain injury.[5] TBI can also be characterized based on mechanism (closed or penetrating head injury) or other features (e.g., occurring in a specific location or over a widespread area).[6] Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.
Traumatic brain injury
Intracranial injury, physically induced brain injury[1]
Physical, cognitive, sensory, social, emotional, and behavioral symptoms
Mild to severe[3]
Trauma to the head[3]
Based on neurological exam, medical imaging[4]
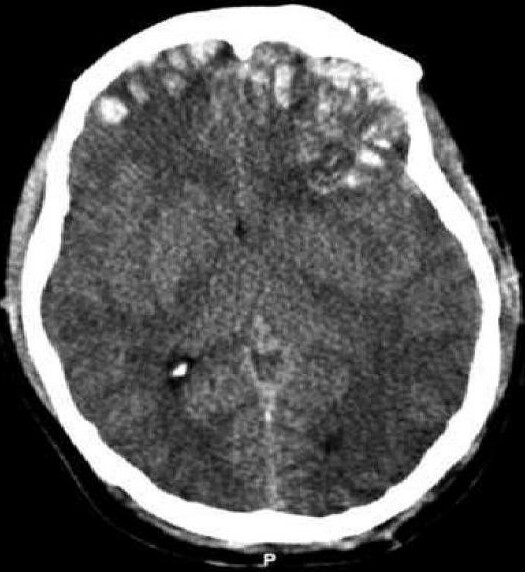
Causes include falls, vehicle collisions and violence. Brain trauma occurs as a consequence of a sudden acceleration or deceleration within the cranium or by a complex combination of both movement and sudden impact. In addition to the damage caused at the moment of injury, a variety of events following the injury may result in further injury. These processes may include alterations in cerebral blood flow and pressure within the skull. Some of the imaging techniques used for diagnosis of moderate to severe TBI include computed tomography (CT) and magnetic resonance imaging (MRIs).
Prevention measures include use of seat belts and helmets, not drinking and driving, fall prevention efforts in older adults and safety measures for children.[7] Depending on the injury, treatment required may be minimal or may include interventions such as medications, emergency surgery or surgery years later. Physical therapy, speech therapy, recreation therapy, occupational therapy and vision therapy may be employed for rehabilitation. Counseling, supported employment and community support services may also be useful.
TBI is a major cause of death and disability worldwide, especially in children and young adults.[8] Males sustain traumatic brain injuries around twice as often as females.[9] The 20th century saw developments in diagnosis and treatment that decreased death rates and improved outcomes.
$_$_$DEEZ_NUTS#0__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#0__subtitleDEEZ_NUTS$_$_$
Research directions
$_$_$DEEZ_NUTS#7__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#7__descriptionDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#1__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#1__descriptionDEEZ_NUTS$_$_$
Causes
The most common causes of TBI in the U.S. include violence, transportation accidents, construction site mishaps, and sports.[42][53] Motor bikes are major causes, increasing in significance in developing countries as other causes reduce.[54][55] The estimates that between 1.6 and 3.8 million traumatic brain injuries each year are a result of sports and recreation activities in the US.[56] In children aged two to four, falls are the most common cause of TBI, while in older children traffic accidents compete with falls for this position.[57] TBI is the third most common injury to result from child abuse.[58] Abuse causes 19% of cases of pediatric brain trauma, and the death rate is higher among these cases.[59] Although men are twice as likely to have a TBI. Domestic violence is another cause of TBI,[60] as are work-related and industrial accidents.[61] Firearms[15] and blast injuries from explosions[62] are other causes of TBI, which is the leading cause of death and disability in war zones.[63] According to Representative Bill Pascrell (Democrat, NJ), TBI is "the signature injury of the wars in Iraq and Afghanistan."[64] There is a promising technology called activation database-guided EEG biofeedback, which has been documented to return a TBI's auditory memory ability to above the control group's performance[65][66]
$_$_$DEEZ_NUTS#3__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#3__descriptionDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#6__descriptionDEEZ_NUTS$_$_$
Prognosis
Prognosis worsens with the severity of injury.[9] Most TBIs are mild and do not cause permanent or long-term disability; however, all severity levels of TBI have the potential to cause significant, long-lasting disability.[140] Permanent disability is thought to occur in 10% of mild injuries, 66% of moderate injuries, and 100% of severe injuries.[141] Most mild TBI is completely resolved within three weeks. Almost all people with mild TBI are able to live independently and return to the jobs they had before the injury, although a small portion have mild cognitive and social impairments.[89] Over 90% of people with moderate TBI are able to live independently, although some require assistance in areas such as physical abilities, employment, and financial managing.[89] Most people with severe closed head injury either die or recover enough to live independently; middle ground is less common.[10] Coma, as it is closely related to severity, is a strong predictor of poor outcome.[11]
Prognosis differs depending on the severity and location of the lesion, and access to immediate, specialised acute management. Subarachnoid hemorrhage approximately doubles mortality.[142] Subdural hematoma is associated with worse outcome and increased mortality, while people with epidural hematoma are expected to have a good outcome if they receive surgery quickly.[76] Diffuse axonal injury may be associated with coma when severe, and poor outcome.[10] Following the acute stage, prognosis is strongly influenced by the patient's involvement in activity that promote recovery, which for most patients requires access to a specialised, intensive rehabilitation service. The Functional Independence Measure is a way to track progress and degree of independence throughout rehabilitation.[143]
Medical complications are associated with a bad prognosis. Examples of such complications include: hypotension (low blood pressure), hypoxia (low blood oxygen saturation), lower cerebral perfusion pressures, and longer times spent with high intracranial pressures.[10][76] Patient characteristics also influence prognosis. Examples of factors thought to worsen it include: abuse of substances such as illicit drugs and alcohol and age over sixty or under two years (in children, younger age at time of injury may be associated with a slower recovery of some abilities).[76] Other influences that may affect recovery include pre-injury intellectual ability, coping strategies, personality traits, family environment, social support systems and financial circumstances.[144]
Life satisfaction has been known to decrease for individuals with TBI immediately following the trauma, but evidence has shown that life roles, age, and depressive symptoms influence the trajectory of life satisfaction as time passes.[145] Many people with traumatic brain injuries have poor physical fitness following their acute injury and this may result with difficulties in day-to-day activities and increased levels of fatigue.[146]
$_$_$DEEZ_NUTS#5__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#5__descriptionDEEZ_NUTS$_$_$
Diagnosis
Quantitative EEG and EEG, which has no specific patterns in TBI is used in research settings to differentiate between mild TBI and no TBI.[192]
Medications
No medication is approved to halt the progression of the initial injury to secondary injury.[63] The variety of pathological events presents opportunities to find treatments that interfere with the damage processes.[10] Although neuroprotection methods to decrease secondary injury have been the subject of interest follows TBI, trials to test agents that could halt these cellular mechanisms have met largely with failure.[10] For example, interest existed in cooling the injured brain; however, a 2020 Cochrane review did not find enough evidence to see if it was useful or not.[193] Maintaining a normal temperature in the immediate period after a TBI appeared useful.[194] One review found a lower than normal temperature was useful in adults but not children.[195] While two other reviews found it did not appear to be useful.[196][194]
Further research is necessary to determine if the vasoconstrictor indomethacin (indometacin) can be used to treat increased pressure in the skull following a TBI.[197] In addition, drugs such as NMDA receptor antagonists to halt neurochemical cascades such as excitotoxicity showed promise in animal trials but failed in clinical trials.[116] These failures could be due to factors including faults in the trials' design or in the insufficiency of a single agent to prevent the array of injury processes involved in secondary injury.[116] Other topics of research have included investigations into mannitol,[103] dexamethasone,[198] progesterone,[199] xenon,[200] barbiturates,[201] magnesium (no strong evidence),[202][203] calcium channel blockers,[204] PPAR-γ agonists,[205][206] curcuminoids,[207] ethanol,[208] NMDA antagonists,[116] caffeine.[209]
Procedures
In addition to traditional imaging modalities, there are several devices that help to monitor brain injury and facilitate research. Microdialysis allows ongoing sampling of extracellular fluid for analysis of metabolites that might indicate ischemia or brain metabolism, such as glucose, glycerol, and glutamate.[210][211] Intraparenchymal brain tissue oxygen monitoring systems (either Licox or Neurovent-PTO) are used routinely in neurointensive care in the US.[212] A non invasive model called CerOx is in development.[213]
Research is also planned to clarify factors correlated to outcome in TBI and to determine in which cases it is best to perform CT scans and surgical procedures.[214]
Hyperbaric oxygen therapy (HBO) has been evaluated as an add on treatment following TBI. The findings of a 2012 Cochrane systematic review does not justify the routine use of hyperbaric oxygen therapy to treat people recovering from a traumatic brain injury.[215] This review also reported that only a small number of randomized controlled trials had been conducted at the time of the review, many of which had methodological problems and poor reporting.[215] HBO for TBI is controversial with further evidence required to determine if it has a role.[216][215]
Psychological
Further research is required to determine the effectiveness of non-pharmacological treatment approaches for treating depression in children/adolescents and adults with TBI.[217]
As of 2010, the use of predictive visual tracking measurement to identify mild traumatic brain injury was being studied. In visual tracking tests, a head-mounted display unit with eye-tracking capability shows an object moving in a regular pattern. People without brain injury are able to track the moving object with smooth pursuit eye movements and correct trajectory. The test requires both attention and working memory which are difficult functions for people with mild traumatic brain injury. The question being studied, is whether results for people with brain injury will show visual-tracking gaze errors relative to the moving target.[218]
Monitoring pressure
Pressure reactivity index is used to correlate intracranial pressure with arterial blood pressure to give information about the state of cerebral perfusion, thus guiding treatment and prevent excessively high or low blood flow to the brain.[219] However, such method of monitoring intracranial pressure of equal or less than 20 mmHg is no better than imaging and clinical examination that monitor the neurological status of the brain in prolonging the survival, preserving the mental or functional status of the subject.[220]
Sensory processing
In animal models of TBI, sensory processing has been widely studied to show systematic defects arise and are slowly but likely only partially recovered.[221] It is especially characterised by an initial period of decreased activity in upper cortical layers.[222][223] This period of decreased activity has also been characterised as by specific timing effects in the patterns of cortical activity in these upper layers in response to regular sensory stimuli.[224]
$_$_$DEEZ_NUTS#6__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#4__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#4__subtextDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#2__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#2__subtextDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#8__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#8__subtextDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#9__titleDEEZ_NUTS$_$_$
$_$_$DEEZ_NUTS#9__subtextDEEZ_NUTS$_$_$