Acute kidney injury
Acute kidney injury (AKI), previously called acute renal failure (ARF),[1][2] is a sudden decrease in kidney function that develops within 7 days,[3] as shown by an increase in serum creatinine or a decrease in urine output, or both.[4]
Acute kidney injury
Acute renal failure (ARF), acute kidney failure (AKF)
Causes of AKI are classified as either prerenal (due to decreased blood flow to the kidney), intrinsic renal (due to damage to the kidney itself), or postrenal (due to blockage of urine flow).[5] Prerenal causes of AKI include sepsis, dehydration, excessive blood loss, cardiogenic shock, heart failure, cirrhosis, and certain medications like ACE inhibitors or NSAIDs.[5] Intrinsic renal causes of AKI include glomerulonephritis, lupus nephritis, acute tubular necrosis, certain antibiotics, and chemotherapeutic agents.[5] Postrenal causes of AKI include kidney stones, bladder cancer, neurogenic bladder, enlargement of the prostate, narrowing of the urethra, and certain medications like anticholinergics.[5]
The diagnosis of AKI is made based on a person's signs and symptoms, along with lab tests for serum creatinine and measurement of urine output. Other tests include urine microscopy and urine electrolytes. Renal ultrasound can be obtained when a postrenal cause is suspected. A kidney biopsy may be obtained when intrinsic renal AKI is suspected and the cause is unclear.[5]
AKI is seen in 10-15% of people admitted to the hospital and in more than 50% of people admitted to the intensive care unit (ICU).[4] AKI may lead to a number of complications, including metabolic acidosis, high potassium levels, uremia, changes in body fluid balance, effects on other organ systems, and death. People who have experienced AKI are at increased risk of developing chronic kidney disease in the future.[4] Management includes treatment of the underlying cause and supportive care, such as renal replacement therapy.
Signs and symptoms[edit]
The clinical presentation is often dominated by the underlying cause. The various symptoms of acute kidney injury result from the various disturbances of kidney function that are associated with the disease. Accumulation of urea and other nitrogen-containing substances in the bloodstream lead to a number of symptoms, such as fatigue, loss of appetite, headache, nausea, and vomiting.[6] Marked increases in the potassium level can lead to abnormal heart rhythms, which can be severe and life-threatening.[7] Fluid balance is frequently affected, though blood pressure can be high, low, or normal.[8]
Pain in the flanks may be encountered in some conditions (such as clotting of the kidneys' blood vessels or inflammation of the kidney). This is the result of stretching of the fibrous tissue capsule surrounding the kidney.[9] If the kidney injury is the result of dehydration, there may be thirst as well as evidence of fluid depletion on physical examination.[9] Physical examination may also provide other clues as to the underlying cause of the kidney problem, such as a rash in interstitial nephritis (or vasculitis) and a palpable bladder in obstructive nephropathy.[9]
Causes[edit]
Prerenal[edit]
Prerenal causes of AKI ("pre-renal azotemia") are those that decrease effective blood flow to the kidney and cause a decrease in the glomerular filtration rate (GFR). Both kidneys need to be affected as one kidney is still more than adequate for normal kidney function. Notable causes of prerenal AKI include low blood volume (e.g., dehydration), low blood pressure, heart failure (leading to cardiorenal syndrome), hepatorenal syndrome in the context of liver cirrhosis, and local changes to the blood vessels supplying the kidney (e.g. NSAID induced vasoconstriction of afferent arteriole). The latter include renal artery stenosis, or the narrowing of the renal artery which supplies the kidney with blood, and renal vein thrombosis, which is the formation of a blood clot in the renal vein that drains blood from the kidney.
Intrinsic or Intrarenal[edit]
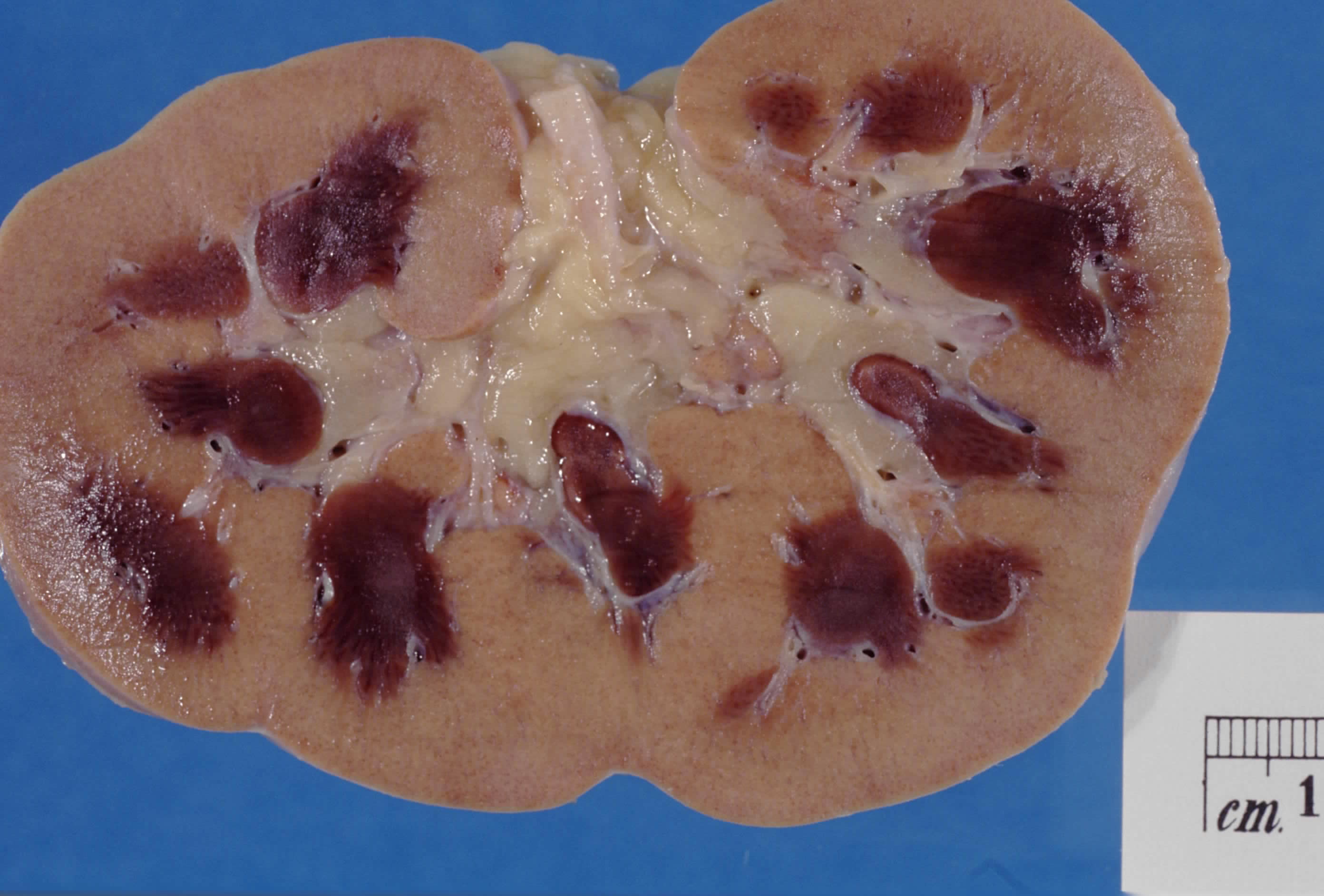
Intrinsic AKI refers to disease processes which directly damage the kidney itself. Intrinsic AKI can be due to one or more of the kidney's structures including the glomeruli, kidney tubules, or the interstitium. Common causes of each are glomerulonephritis, acute tubular necrosis (ATN), and acute interstitial nephritis (AIN), respectively. Other causes of intrinsic AKI are rhabdomyolysis and tumor lysis syndrome.[10] Certain medication classes such as calcineurin inhibitors (e.g., tacrolimus) can also directly damage the tubular cells of the kidney and result in a form of intrinsic AKI.[11]
Postrenal[edit]
Postrenal AKI refers to acute kidney injury caused by disease states downstream of the kidney and most often occurs as a consequence of urinary tract obstruction. This may be related to benign prostatic hyperplasia, kidney stones, obstructed urinary catheter, bladder stones, or cancer of the bladder, ureters, or prostate.
Prognosis[edit]
Mortality[edit]
Mortality after AKI remains high. AKI has a death rate as high as 20%, which may reach up to 50% in the intensive care unit (ICU). Each year, around two million people die of AKI worldwide.[37]
AKI develops in 5% to 30% of patients who undergo cardiothoracic surgery, depending on the definition used for AKI.[38] If AKI develops after major abdominal surgery (13.4% of all people who have undergone major abdominal surgery) the risk of death is markedly increased (over 12-fold).[39]
Kidney function[edit]
Depending on the cause, a proportion of patients (5–10%) will never regain full kidney function, thus entering end-stage kidney failure and requiring lifelong dialysis or a kidney transplant. Patients with AKI are more likely to die prematurely after being discharged from hospital, even if their kidney function has recovered.[2]
The risk of developing chronic kidney disease is increased (8.8-fold).[40]
Epidemiology[edit]
New cases of AKI are unusual but not rare, affecting approximately 0.1% of the UK population per year (2000 ppm/year), 20x incidence of new ESKD (end-stage kidney disease). AKI requiring dialysis (10% of these) is rare (200 ppm/year), 2x incidence of new ESKD.[41]
There is an increased incidence of AKI in agricultural workers because of occupational hazards such as dehydration and heat illness.[42] No other traditional risk factors, including age, BMI, diabetes, or hypertension, were associated with incident AKI.
Acute kidney injury is common among hospitalized patients. It affects some 3–7% of patients admitted to the hospital and approximately 25–30% of patients in the intensive care unit.[43]
Acute kidney injury was one of the most expensive conditions seen in U.S. hospitals in 2011, with an aggregated cost of nearly $4.7 billion for approximately 498,000 hospital stays.[44] This was a 346% increase in hospitalizations from 1997, when there were 98,000 acute kidney injury stays.[45] According to a review article of 2015, there has been an increase in cases of acute kidney injury in the last 20 years which cannot be explained solely by changes to the manner of reporting.[46]
History[edit]
Before the advancement of modern medicine, acute kidney injury was referred to as uremic poisoning while uremia was contamination of the blood with urine. Starting around 1847, uremia came to be used for reduced urine output, a condition now called oliguria, which was thought to be caused by the urine's mixing with the blood instead of being voided through the urethra.[47]
Acute kidney injury due to acute tubular necrosis (ATN) was recognized in the 1940s in the United Kingdom, where crush injury victims during the London Blitz developed patchy necrosis of kidney tubules, leading to a sudden decrease in kidney function.[48] During the Korean and Vietnam wars, the incidence of AKI decreased due to better acute management and administration of intravenous fluids.[49]