COVID-19 vaccination in the United Kingdom
The COVID-19 vaccination programme in the United Kingdom is an ongoing mass immunisation campaign for coronavirus disease 2019 (COVID-19) during the COVID-19 pandemic in the United Kingdom.
Date
8 December 2020 – present
United Kingdom
Immunisation of the public in the United Kingdom against COVID-19
53,710,109 have received one vaccine dose
50,483,527 have received two vaccine doses
40,196,024 have received three vaccine doses,
6,200,537 have received a fourth dose[1]
92.9% of UK population 12+ have received one vaccine dose
86.8% of UK population 12+ have received two vaccine doses
69% of UK population 12+ have received three vaccine doses[1]
Vaccinations began on 8 December 2020 after Margaret Keenan became the first person in the world (outside trials) to receive her first dose of two of the Pfizer–BioNTech COVID-19 vaccine.[2] There are three vaccines currently in use; following approval of the Pfizer–BioNTech COVID-19 vaccine (Comirnaty), vaccines developed by University of Oxford and AstraZeneca (Vaxzevria), and the United States National Institute of Allergy and Infectious Diseases and Moderna (Spikevax) have been rolled out. As of 13 September 2021, there were four other COVID-19 vaccines on order for the programme, at varying stages of development.
Phase 1 of the rollout prioritised the most vulnerable, in a schedule primarily based on age. The delivery plan was adjusted on 30 December 2020, delaying second doses so that more people could receive their first dose. A target to give all 15 million people in the top four priority groups their first dose by the middle of February 2021 was announced on 4 January 2021, and achieved on 14 February 2021. The next five groups were offered a vaccine by 15 April, and 32 million doses were administered by that point. In June 2021, all adults aged 18+ were able to get their first dose of a vaccine. The vaccine rollout was expanded to adolescent children and booster doses during the later months of that year.[3] In response to the SARS-CoV-2 Omicron variant, third vaccine doses were made available to all adults in December 2021.[4]
The UK's rollout was among the fastest in the world with among the highest uptake in its first few months,[2] although vaccination rates had slowed down or plateaued by autumn 2021 due to lower uptake in younger age groups.[5][6] Polling suggests the UK's level of COVID-19 vaccine hesitancy is among the world's lowest.[7][8]
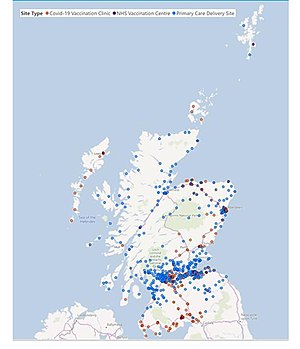
Vaccination sites include GP practices, care homes and pharmacies, as well as hospitals. As of 21 May 2021, there were 2,057 vaccination sites operating in England.[9] There are over 1,100 vaccination sites operating in Scotland.[10] As of 25 May 2021, there were 462 vaccination sites operating in Wales.[11] Additional sites, including large venues such as sports stadia, entered the programme from 11 January 2021, with seven mass vaccination centres opening in England initially and seven in Wales.[12]
New guidance for allergy sufferers, antibody tests, new variants of SARS-CoV-2 (B.1.1.7 and B.1.617) and the use of the AstraZeneca vaccine in younger adults have been issued throughout the programme.
The programme also includes procurement of vaccines for British Overseas Territories and Crown Dependencies.[13][14]
According to a June 2022 study published in The Lancet, COVID-19 vaccination in the United Kingdom prevented an additional 507,000 deaths from December 8, 2020 to December 8, 2021.[15][16]
Background[edit]
Responsibility for deployment[edit]
On 28 November 2020 the new role of Parliamentary Under-Secretary of State for COVID-19 Vaccine Deployment was set up within the Department of Health and Social Care in the Government of the United Kingdom, with Nadhim Zahawi the first to take office.[22]
Vaccines on order[edit]
There are several COVID-19 vaccines at various stages of development around the world. By February 2021 the British Government had placed orders for a combined total of 457 million doses across 8 different vaccines,[23][24][25][26] and as of 23 August 2021 this had increased to more than 540 million doses.[27] This does not equate to the number of people that can be immunised as most vaccines require more than one dose.
In September 2021, the UK government cancelled their 190-million-dose Valneva order, citing supply concerns.[28]
The breakdown of the vaccines currently being considered for the vaccination programme is as follows:[29][30]
History[edit]
Regulatory approvals[edit]
On 2 December 2020, the UK became the first country to give approval for use of the Pfizer–BioNTech vaccine,[36][37] later branded as Comirnaty.[38] This was in the form of a temporary authorisation given by the Medicines and Healthcare products Regulatory Agency (MHRA) under Regulation 174 of the Human Medicines Regulations 2012.[39] Regulatory approval is reserved under the devolution settlement. The first batch arrived in the UK the next day and was initially stored at an undisclosed central hub before being distributed to hospital vaccination centres across the country.[40]
On 30 December 2020, the UK also became the first country to approve the Oxford/AstraZeneca vaccine.[31]
On 8 January 2021, the Moderna vaccine was approved as the third vaccine to enter the programme.[24]
On 28 January 2021, the results of the Novavax vaccine trials, which were undertaken in the UK and in South Africa, showed it was 95.6% effective against the original SARS-CoV-2 strains and 85.6% against the Variant of Concern 202012/01, then prevalent in the UK. The company stated it had begun the process of requesting clearance for use in the UK.[41] The Novavax vaccine was the first to be tested in clinical trials for efficacy against the UK's prevailing Variant of Concern 202012/01.[42] In clinical trial subjects without HIV infections, the vaccine was also 60% effective against the 501.V2 variant, a SARS-CoV-2 strain first detected in South Africa.[42]
On 28 May 2021, the Janssen vaccine was the fourth vaccine to be approved in the UK.[34]
On 3 February 2022, the Novavax vaccine was the fifth vaccine to be approved in the UK.[35]
On 14 April 2022, the UK became the first country to approve the Valneva vaccine. This is the sixth COVID-19 vaccine that the MHRA has approved.[43]
Rollout timeline[edit]
This timeline lists the general availability of vaccine appointments in England, by date. The dates differed slightly in Scotland, Wales and Northern Ireland (not listed here).
Companies and organisations involved[edit]
In the months before approval of the first vaccine, the Joint Committee on Vaccination and Immunisation (an independent group of experts) gave advice to the Vaccine Taskforce on the groups of people that should be prioritised for vaccination.[79][80] The taskforce was formed in May 2020 to lead efforts to develop, manufacture and procure vaccines for the UK and globally,[81] and was led until the end of 2020 by biotech venture capital manager Kate Bingham.[82]
As with other licensed vaccines, the National Institute for Biological Standards and Control (part of the MHRA) reviews the production process and the manufacturer's quality control, and tests each batch of vaccine.[83] Again in common with other vaccines and medicines, the MHRA monitors adverse reactions by collecting details submitted by healthcare workers, carers and the public through the Yellow Card Scheme; the agency set up a web reporting site specific to the COVID-19 vaccines.[84]
The creation of the Vaccines Manufacturing and Innovation Centre was announced in December 2018, to provide the UK with a vaccine development and manufacturing facility, and its building is under construction at Harwell with planned completion brought forward from 2022 to 2021. The academic/industrial consortium assisted with development and early production of the Oxford–AstraZeneca vaccine during 2020.[85] Services contractor Serco has a role in the deployment, as part of a contract which was extended for six months in June 2021 at a cost of £424 million.[86]
The British Armed Forces have assisted with the vaccine rollout through the COVID Support Force in all parts of the UK. This has involved assistance with planning, the construction of vaccination centres and the contribution of staff to administer vaccines. This support is provided through the provisions of the military aid to the civil authorities (MACA) mechanism and is part of the military's wider contribution under Operation Rescript.[87]