Inflammatory bowel disease
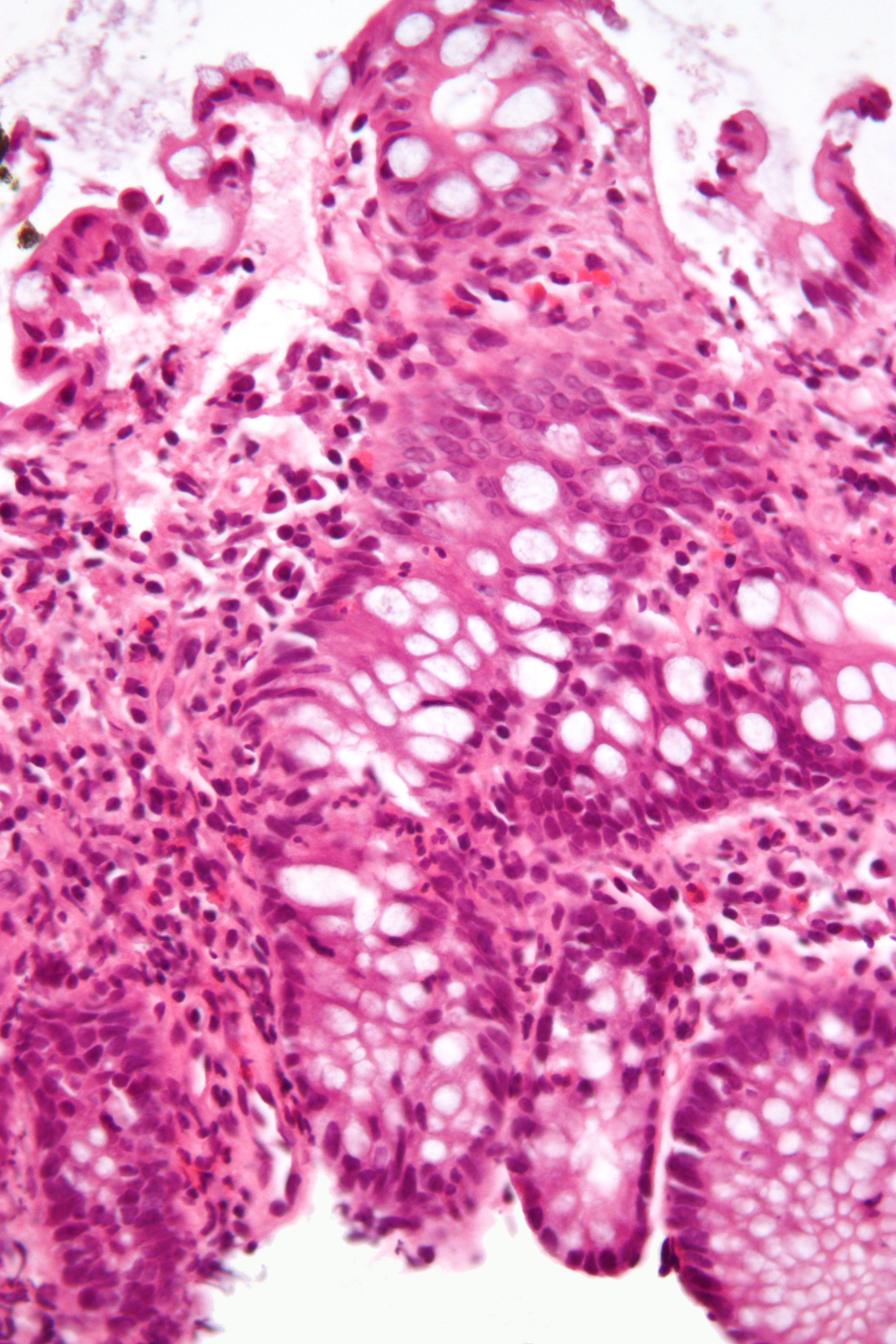
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types.[3] Crohn's disease affects the small intestine and large intestine, as well as the mouth, esophagus, stomach and the anus, whereas UC primarily affects the colon and the rectum.[4][5][6]
This article is about bowel inflammation. For the functional disorder, see Irritable bowel syndrome. For the medical journal, see Inflammatory Bowel Diseases.Treatment standards[edit]
Crohn's and Colitis Australia, the peak body for IBD in Australia, where prevalence is one of the highest in the world, reviewed the quality of care for patients admitted to Australian hospitals. They found that only one hospital met accepted standards for multidisciplinary care, but that care was improved with the availability of even minimal specialised services.[104]
Epidemiology[edit]
IBD resulted in a global total of 51,000 deaths in 2013 and 55,000 deaths in 1990.[119] The increased incidence of IBD since World War II has been correlated to the increase in meat consumption worldwide, supporting the claim that animal protein intake is associated with IBD.[120] However, there are many environmental risk factors that have been linked to the increased and decreased risk of IBD, such as smoking, air pollution and greenspace, urbanization and Westernization.[121] Inflammatory bowel diseases are increasing in Europe.[122] Incidence and prevalence of IBD has risen steadily for the last decades in Asia, which could be related changes in diet and other environmental factors.[123]
Around 0.8% of people in the UK have IBD.[124] Similarly, around 270,000 (0.7%) of people in Canada have IBD,[125] with that number expected to rise to 400,000 (1%) by 2030.[126]
Research[edit]
The following treatment strategies are not used routinely, but appear promising in some forms of IBD.
Initial reports[127] suggest that helminthic therapy may not only prevent but even control IBD: a drink with roughly 2,500 ova of the Trichuris suis helminth taken twice monthly decreased symptoms markedly in many patients. It is even speculated that an effective "immunization" procedure could be developed—by ingesting the cocktail at an early age.[128]
Prebiotics and probiotics are focusing increasing interest as treatments for IBD. Currently, there is evidence to support the use of certain probiotics in addition to standard treatments in people with ulcerative colitis but there is no sufficient data to recommend probiotics in people with Crohn's disease. Both single strain and multi-strain probiotics have been researched for mild to moderate cases of ulcerative colitis. The most clinically researched multi-strain probiotic with over 70 human trials is the De Simone Formulation.[129] Further research is required to identify specific probiotic strains or their combinations and prebiotic substances for therapies of intestinal inflammation.[130]
Currently, the probiotic strain, frequency, dose and duration of the probiotic therapy are not established.[131] In severely ill people with IBD there is a risk of the passage of viable bacteria from the gastrointestinal tract to the internal organs (bacterial translocation) and subsequent bacteremia, which can cause serious adverse health consequences.[131] Live bacteria might not be essential because of beneficial effects of probiotics seems to be mediated by their DNA and by secreted soluble factors, and their therapeutic effects may be obtained by systemic administration rather than oral administration.[131][132]
In 2005 New Scientist published a joint study by Bristol University and the University of Bath on the apparent healing power of cannabis on IBD. Reports that cannabis eased IBD symptoms indicated the possible existence of cannabinoid receptors in the intestinal lining, which respond to molecules in the plant-derived chemicals. CB1 cannabinoid receptors – which are known to be present in the brain – exist in the endothelial cells which line the gut, it is thought that they are involved in repairing the lining of the gut when damaged.[133]
The team deliberately damaged the cells to cause inflammation of the gut lining and then added synthetically produced cannabinoids; the result was that gut started to heal: the broken cells were repaired and brought back closer together to mend the tears. It is believed that in a healthy gut, natural endogenous cannabinoids are released from endothelial cells when they are injured, which then bind to the CB1 receptors. The process appears to set off a wound-healing reaction, and when people use cannabis, the cannabinoids bind to these receptors in the same way.[133]
Previous studies have shown that CB1 receptors located on the nerve cells in the gut respond to cannabinoids by slowing gut motility, therefore reducing the painful muscle contractions associated with diarrhea. CB2, another cannabinoid receptor predominantly expressed by immune cells, was detected in the gut of people with IBD at a higher concentration. These receptors, which also respond to chemicals in cannabis, appear to be associated with apoptosis – programmed cell death – and may have a role in suppressing the overactive immune system and reducing inflammation by mopping up excess cells.[133]
Activation of the endocannabinoid system was found efficient in ameliorating colitis and increasing the survival rate of mice, and reducing remote organ changes induced by colitis, further suggest that modulation of this system is a potential therapeutic approach for IBDs and the associated remote organ lesions.[134]
Alicaforsen is a first generation antisense oligodeoxynucleotide designed to bind specifically to the human ICAM-1 messenger RNA through Watson-Crick base pair interactions in order to subdue expression of ICAM-1.[135] ICAM-1 propagates an inflammatory response promoting the extravasation and activation of leukocytes (white blood cells) into inflamed tissue.[135] Increased expression of ICAM-1 has been observed within the inflamed intestinal mucosa of people with ulcerative colitis, pouchitis and Crohn's, where ICAM-1 over production correlated with disease activity.[136] This suggests that ICAM-1 is a potential therapeutic target in the treatment of these diseases.[137][138]
Cannabinoid CB2 receptor agonists are found to decrease the induction of ICAM-1 and VCAM-1 surface expression in human brain tissues and primary human brain endothelial cells (BMVEC) exposed to various pro-inflammatory mediators.[139]
In 2014, an alliance among the Broad Institute, Amgen and Massachusetts General Hospital formed with the intention to "collect and analyze patient DNA samples to identify and further validate genetic targets."[140]
In 2015, a meta-analysis on 938 IBD patients and 953 controls, IBD was significantly associated with having higher odds of vitamin D deficiency.[141]
Gram-positive bacteria present in the lumen could be associated with extending the time of relapse for ulcerative colitis.[130]
Bidirectional pathways between depression and IBD have been suggested [142] and psychological processes have been demonstrated to influence self-perceived physical and psychological health over time.[143] IBD-disease activity may impact quality of life and over time may significantly affect individual's mental well-being, which may be related to the increased risk to develop anxiety and/or depression.[142][144][145] On the other hand, psychological distress may also influence IBD activity.[146]
Higher rates of anxiety and depression are observed among those with IBD compared to healthy individuals, which correlated with disease severity.[144][146] Part of this phenotypic correlation is due to a shared genetic overlap between IBD and psychiatric comorbidities.[147] Moreover, anxiety and depression rates increase during active disease compared with inactive phases.[146]
In other species[edit]
IBD also occurs in dogs and is thought to arise from a combination of host genetics, intestinal microenvironment, environmental components and the immune system. There is an ongoing discussion, however, that the term "chronic enteropathy" might be better to use than "inflammatory bowel disease" in dogs because it differs from IBD in humans in how the dogs respond to treatment. For example, many dogs respond to only dietary changes compared to humans with IBD, who often need immunosuppressive treatment. Some dogs may also need immunosuppressant or antibiotic treatment when dietary changes are not enough. After having excluded other diseases that can lead to vomiting, diarrhea, and abdominal pain in dogs, intestinal biopsies are often performed to investigate what kind of inflammation is occurring (lymphoplasmacytic, eosinophilic, or granulomatous). In dogs, low levels of cobalamin in the blood have been shown to be a risk factor for negative outcome.[148][149][150]