Seizure
A seizure is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain.[6] Outward effects vary from uncontrolled shaking movements involving much of the body with loss of consciousness (tonic-clonic seizure), to shaking movements involving only part of the body with variable levels of consciousness (focal seizure), to a subtle momentary loss of awareness (absence seizure).[3] These episodes usually last less than two minutes and it takes some time to return to normal.[5][8] Loss of bladder control may occur.[3]
This article is about epileptic seizures. For other types of seizures, see Non-epileptic seizure. For other uses, see Seizure (disambiguation).Epileptic seizure
Variable[3]
Falling, drowning, car accidents, pregnancy complications, emotional health issues[4]
Typically < 2 minutes[5]
Focal, generalized; Provoked, unprovoked[6]
Provoked: Low blood sugar, alcohol withdrawal, low blood sodium, fever, brain infection, traumatic brain injury[3][6]
Unprovoked: Unknown, brain injury, brain tumor, previous stroke[5][3][6][7]
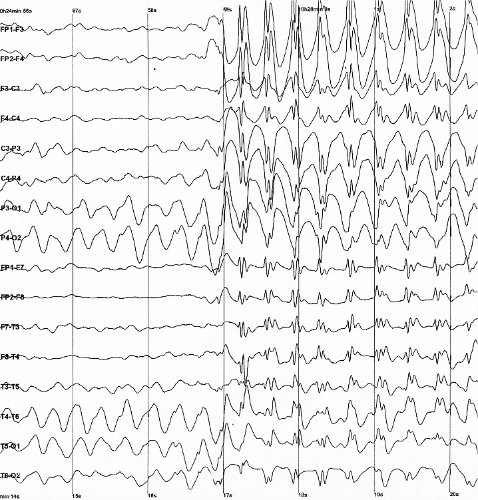
Based on symptoms, blood tests, medical imaging, electroencephalography[7]
Less than 5 min: Place person on their side, remove nearby dangerous objects[8]
More than 5 min: Treat as per status epilepticus[8]
Seizures may be provoked and unprovoked.[6] Provoked seizures are due to a temporary event such as low blood sugar, alcohol withdrawal, abusing alcohol together with prescription medication, low blood sodium, fever, brain infection, flashing images or concussion.[3][6] Unprovoked seizures occur without a known or fixable cause such that ongoing seizures are likely.[5][3][6][7] Unprovoked seizures may be exacerbated by stress or sleep deprivation.[3] Epilepsy describes a brain disease in which there has been at least one unprovoked seizure and where there is a high risk of additional seizures in the future.[6] Conditions that look like epileptic seizures but are not include: fainting, nonepileptic psychogenic seizure and tremor.[3]
A seizure that lasts for more than a brief period is a medical emergency.[10] Any seizure lasting longer than five minutes should be treated as status epilepticus.[8] A first seizure generally does not require long-term treatment with anti-seizure medications unless a specific problem is found on electroencephalogram (EEG) or brain imaging.[7] Typically it is safe to complete the work-up following a single seizure as an outpatient.[3] In many, with what appears to be a first seizure, other minor seizures have previously occurred.[11]
Up to 10% of people have had at least one epileptic seizure in their lifetime.[5][9] Provoked seizures occur in about 3.5 per 10,000 people a year while unprovoked seizures occur in about 4.2 per 10,000 people a year.[5] After one seizure, the chance of experiencing a second one is about 40%.[12][13] Epilepsy affects about 1% of the population at any given time.[9]
Any animal that has a brain can have a seizure.[14]
Mechanism[edit]
Normally, brain electrical activity is non-synchronous.[19] In epileptic seizures, due to problems within the brain,[45] a group of neurons begin firing in an abnormal, excessive,[16] and synchronized manner.[19] This results in a wave of depolarization known as a paroxysmal depolarizing shift.[46]
Normally after an excitatory neuron fires it becomes more resistant to firing for a period of time.[19] This is due in part from the effect of inhibitory neurons, electrical changes within the excitatory neuron, and the negative effects of adenosine.[19] In epilepsy the resistance of excitatory neurons to fire during this period is decreased.[19] This may occur due to changes in ion channels or inhibitory neurons not functioning properly.[19] Forty-one ion-channel genes and over 1,600 ion-channel mutations have been implicated in the development of epileptic seizure.[47] These ion channel mutations tend to confer a depolarized resting state to neurons resulting in pathological hyper-excitability.[48] This long-lasting depolarization in individual neurons is due to an influx of Ca2+ from outside of the cell and leads to extended opening of Na+ channels and repetitive action potentials.[49] The following hyperpolarization is facilitated by γ-aminobutyric acid (GABA) receptors or potassium (K+) channels, depending on the type of cell.[49] Equally important in epileptic neuronal hyper-excitability is the reduction in the activity of inhibitory GABAergic neurons, an effect known as disinhibition. Disinhibition may result from inhibitory neuron loss, dysregulation of axonal sprouting from the inhibitory neurons in regions of neuronal damage, or abnormal GABAergic signaling within the inhibitory neuron.[50] Neuronal hyper-excitability results in a specific area from which seizures may develop, known as a "seizure focus".[19] Following an injury to the brain, another mechanism of epilepsy may be the up regulation of excitatory circuits or down regulation of inhibitory circuits.[19][51] These secondary epilepsies occur through processes known as epileptogenesis.[19][51] Failure of the blood–brain barrier may also be a causal mechanism.[52] While blood-brain barrier disruption alone does appear to cause epileptogenesis, it has been correlated to increased seizure activity.[53] Furthermore, it has been implicated in chronic epileptic conditions through experiments inducing barrier permeability with chemical compounds.[53] Disruption may lead to fluid leaking out of the blood vessels into the area between cells and driving epileptic seizures.[54] Preliminary findings of blood proteins in the brain after a seizure support this theory.[53]
Focal seizures begin in one hemisphere of the brain while generalized seizures begin in both hemispheres.[21] Some types of seizures may change brain structure, while others appear to have little effect.[55] Gliosis, neuronal loss, and atrophy of specific areas of the brain are linked to epilepsy but it is unclear if epilepsy causes these changes or if these changes result in epilepsy.[55]
Seizure activity may be propagated through the brain's endogenous electrical fields.[56] Proposed mechanisms that may cause the spread and recruitment of neurons include an increase in K+ from outside the cell,[57] and increase of Ca2+ in the presynaptic terminals.[49] These mechanisms blunt hyperpolarization and depolarizes nearby neurons, as well as increasing neurotransmitter release.[49]
Prevention[edit]
A number of measures have been attempted to prevent seizures in those at risk. Following traumatic brain injury anticonvulsants decrease the risk of early seizures but not late seizures.[70]
In those with a history of febrile seizures, some medications (both antipyretics and anticonvulsants) have been found effective for reducing reoccurrence, however due to the frequency of adverse effects and the benign nature of febrile seizures the decision to use medication should be weighted carefully against potential negative effects.[71]
There is no clear evidence that antiepileptic drugs are effective or not effective at preventing seizures following a craniotomy,[72] following subdural hematoma,[73] after a stroke,[74][75] or after subarachnoid haemorrhage,[76] for both people who have had a previous seizure, and those who have not.
Prognosis[edit]
Following a first seizure, the risk of more seizures in the next two years is around 40%.[12][13] The greatest predictors of more seizures are problems either on the electroencephalogram or on imaging of the brain.[7] In adults, after 6 months of being seizure-free after a first seizure, the risk of a subsequent seizure in the next year is less than 20% regardless of treatment.[89] Up to 7% of seizures that present to the emergency department (ER) are in status epilepticus.[58] In those with a status epilepticus, mortality is between 10% and 40%.[15] Those who have a seizure that is provoked (occurring close in time to an acute brain event or toxic exposure) have a low risk of re-occurrence, but have a higher risk of death compared to those with epilepsy.[90]
Epidemiology[edit]
Approximately 8–10% of people will experience an epileptic seizure during their lifetime.[91] In adults, the risk of seizure recurrence within the five years following a new-onset seizure is 35%; the risk rises to 75% in persons who have had a second seizure.[91] In children, the risk of seizure recurrence within the five years following a single unprovoked seizure is about 50%; the risk rises to about 80% after two unprovoked seizures.[92] In the United States in 2011, seizures resulted in an estimated 1.6 million emergency department visits; approximately 400,000 of these visits were for new-onset seizures.[91] The exact incidence of epileptic seizures in low-income and middle-income countries is unknown, however it probably exceeds that in high-income countries.[93] This may be due to increased risks of traffic accidents, birth injuries, and malaria and other parasitic infections.[93]
History[edit]
Epileptic seizures were first described in an Akkadian text from 2000 B.C.[94] Early reports of epilepsy often saw seizures and convulsions as the work of "evil spirits".[95] The perception of epilepsy, however, began to change in the time of Ancient Greek medicine. The term "epilepsy" itself is a Greek word, which is derived from the verb "epilambanein", meaning "to seize, possess, or afflict".[94] Although the Ancient Greeks referred to epilepsy as the "sacred disease", this perception of epilepsy as a "spiritual" disease was challenged by Hippocrates in his work On the Sacred Disease, who proposed that the source of epilepsy was from natural causes rather than supernatural ones.[95]
Early surgical treatment of epilepsy was primitive in Ancient Greek, Roman and Egyptian medicine.[96] The 19th century saw the rise of targeted surgery for the treatment of epileptic seizures, beginning in 1886 with localized resections performed by Sir Victor Horsley, a neurosurgeon in London.[95] Another advancement was that of the development by the Montreal procedure by Canadian neurosurgeon Wilder Penfield, which involved use of electrical stimulation among conscious patients to more accurately identify and resect the epileptic areas in the brain.[95]
Society and culture[edit]
Economics[edit]
Seizures result in direct economic costs of about one billion dollars in the United States.[7] Epilepsy results in economic costs in Europe of around €15.5 billion in 2004.[16] In India, epilepsy is estimated to result in costs of US$1.7 billion or 0.5% of the GDP.[45] They make up about 1% of emergency department visits (2% for emergency departments for children) in the United States.[30]
Research[edit]
Scientific work into the prediction of epileptic seizures began in the 1970s. Several techniques and methods have been proposed, but evidence regarding their usefulness is still lacking.[97]
Two promising areas include gene therapy,[98] and seizure detection and seizure prediction.[99]
Gene therapy for epilepsy consists of employing vectors to deliver pieces of genetic material to areas of the brain involved in seizure onset.[98]
Seizure prediction is a special case of seizure detection in which the developed systems is able to issue a warning before the clinical onset of the epileptic seizure.[97][99]
Computational neuroscience has been able to bring a new point of view on the seizures by considering the dynamical aspects.[61]